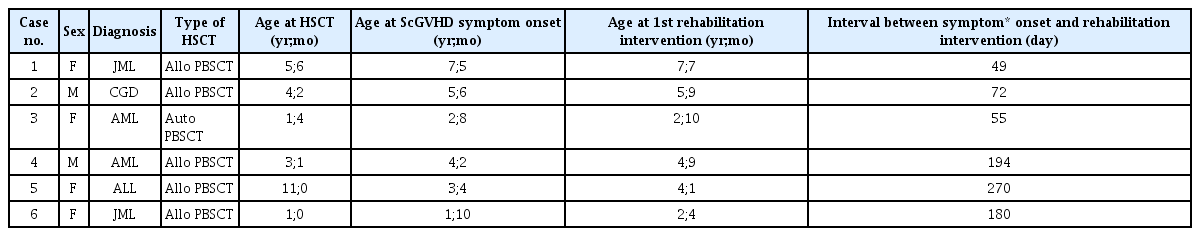
Rehabilitation in Children With Sclerodermoid Chronic Graft-Versus-Host Disease: Case Series
Article information
Abstract
Joint contracture in chronic graft-versus-host disease (cGVHD) is refractory to treatment, and tends to deteriorate gradually over time. There is scant clinical research focusing on timing and intensity of rehabilitation on joint contractures in children with sclerodermoid cGVHD after hematopoietic stem cell transplantation. We retrospectively reviewed rehabilitative therapeutic effects in 6 children with sclerodermoid cGVHD, whose clinical records documented their condition, before and after rehabilitation therapies. Three children who started treatment within a mean of 2 months after the onset of joint symptoms, and who underwent home-based exercise twice daily for 30 minutes showed more prominent improvement in range of motion compared with the other 3 children, who started rehabilitation therapy later than 6 months after onset of joint symptoms, without regular home-based exercise.
INTRODUCTION
Allogeneic hematopoietic stem cell transplantation (HSCT), has been performed to treat many hematologic diseases. Acute and chronic graft-versus-host disease (GVHD) are multisystem disorders that are common complications of allogeneic HSCT. Chronic GVHD (cGVHD) is the most common long-term complication after allogeneic HSCT; and is a major cause of late morbidity that impairs quality of life and function [1]. While acute GVHD is driven mainly by mature donor T cells, cGVHD involves a more complex immune reaction with T and B cells contributing to underlying pathology [2]. Although donor antibodies to recipient antigens play a role in cGVHD, exact mechanisms of how these cells contribute to underlying pathology are being investigated. BAFF is a key regulator of B-cell homeostasis, and high levels have been shown to rescue self-reactive B cells from peripheral deletion [3] promoting survival and differentiation.
Among the symptoms of cGVHD, sclerodermoid GVHD (ScGVHD) is a major risk factor for joint contractures and related pain and dysfunction, and results from inflammation and fibrosis (Fig. 1) of the dermis, subcutaneous tissue, or fascia [2]. Clinically, sclerodermatous GVHD often shows a rippled skin appearance, whereas fasciitis may present with stone-like tightness on palpation and lucidity of overlying skin. In histopathological examinations of fasciitis, oedema and fibrosis are confined to the fasciae and subcutaneous septa with entrapment of subcutaneous fat and a pericapillary lymphoplasmacellular infiltrate [4]; these changes result in reduced range of motion (ROM), and significant loss of strength and functional capabilities.

Appearance of the affected extremities in patient with sclerodermoid chronic graft-versus-host disease.
Although ScGVHD is a disabling disease causing functional impairment and decreased quality of life, there are no studies addressing the critical nature of early initiation of rehabilitation therapy or home-based exercise [5]. Hence, we illustrate the critical nature of timing of rehabilitative intervention after symptom onset in children with ScGVHD, and the importance of regular homebased exercise.
CASE REPORTS
According to medical records of the Asan Medical Center of Seoul, Korea, 91 pediatric patients (younger than age 18) diagnosed with cGVHD, were referred to the Department of Rehabilitation Medicine, Division of Pediatric Rehabilitation Medicine for rehabilitation therapy 1997–2017. Among them, we identified 6 children affected by ScGVHD after HSCT, for whom we identified preand post-rehabilitation therapy assessments. Average age of the study population was 5.8 years, when rehabilitation was first initiated. Diagnoses and joints affected are presented in Tables 1 and 2. These 6 children with significant joint contractures participated in a rehabilitation therapy program, including physical therapy such as stretching exercises to improve ROM and occupational therapy to increase ROM and prevent disuse atrophy. We provided an education session for the parents to teach them how to continue stretching their children’s affected joints.
Three of the children showed significant improvement, while the other three did not show significant improvement or change in ROM. The differences depended on the time to initiate rehabilitation after ScGVHD, and intensity of home-based exercise. Three children who started treatment within a mean of 2 months after the onset of joint symptoms, and who underwent home-based exercise twice a day for 30 minutes, showed more prominent improvement in ROM, compared with the other 3 children who started rehabilitation therapy later than 6 months after the onset of joint symptoms without regular home-based exercise.
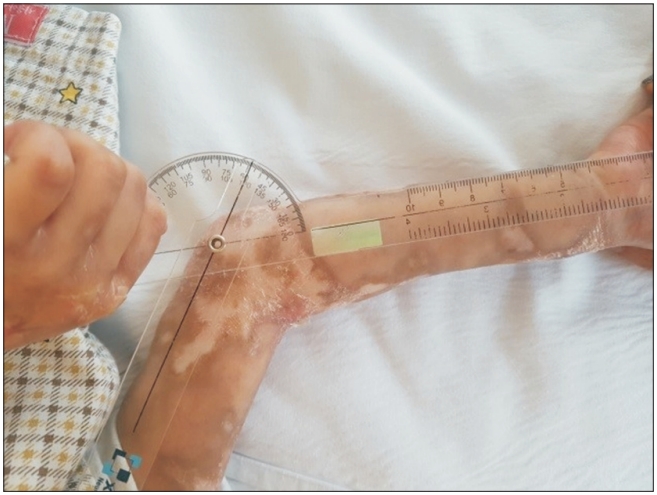
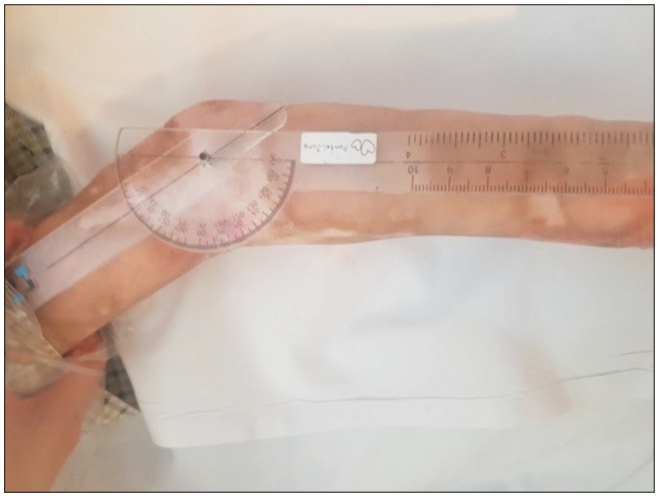
Case 1, 2, and 3
Characteristics of children are presented in Table 1. They were referred to clinic for rehabilitation therapy mean 58.6 days (49 days for case 1, 72 days for case 2, and 55 days for case 3) after their symptoms of joint contracture were diagnosed. We instructed the parents to exercise their child, twice a day for 30 minutes. In the case 1 child, after five sessions of rehabilitation therapy and home-based exercise including ROM exercise, her elbow extension surprisingly improved to -30° on the right (Figs. 2, 3). In the case 2 child, after faithfully maintaining the home exercise program. Surprisingly, the right wrist extension angle improved by 75° and the right MCP joint flexion also improved by 75° after only 2 weeks of passive ROM exercise. In the case 3 child, the joint contractures on both wrists and right PIP joints improved to completely normal from intensive and active home-based exercise of the wrists for 7 months and of the IP joints for 16 months.
Case 4, 5, and 6
Characteristics of children are presented in Table 1. They were referred to clinic for rehabilitation therapy mean 214.6 days (194 days for case 1, 270 days for case 2, and 180 days for case 3), after their symptoms of joint contracture were diagnosed. They did not show significant improvement in ROM home-based exercise. They were treated at the hospital for 30 minutes once a week, and treatment duration varied from 3 months for case 5 to 40 months for case 6. Home-based exercise therapy was not performed due to lack of parental cooperation.
DISCUSSION
Although effectiveness of rehabilitation therapy has been reported, it is the first study to confirm effectiveness of rehabilitation according to the timing of rehabilitation after ScGVHD symptom onset in children younger than age 10. Although this is not a case control study, degree of improvement in ROM was significantly greater than a previous study [5] in patients who underwent rehabilitation treatment within a mean of 60 days after ScGVHD symptom onset. Those results may due to applying intensive rehabilitation before the onset of definite joint contracture and regular home-based exercise twice daily.
Physical rehabilitation in cGVHD can facilitate restoration of musculoskeletal system function, which would allow patients to retain some mobility and independence [6]. Once a contracture has developed active and passive ROM exercises with sustained stretch at least twice daily are necessary [7]. Home-based exercise is essential to perform frequent joint exercises, and it is crucial for parents to conduct regular joint range exercise to prevent joint contracture [8].
In terms of immunosuppressive agents and steroids, standard initial therapy of cGVHD is prednisone with or without a calcineurin inhibitor, although only approximately 50% of persons have durable response [9]. Immunosuppressive agents including sirolimus, tacrolimus, mycophenolate, methotrexate are recommended but poorly standardized as standard next therapy [10]. There were only drugs continuously used before ScGVHD symptom manifestation without adding or increasing dosage during rehabilitation therapy (Table 2).
ScGVHD may have lengthy contracting duration with progressive sclerotic changes and cause multiple joint contractures. Therefore, we suggest that ScGVHD patients are managed with aggressive rehabilitation therapy from onset of the illness and maintain therapy for an extended time to restore joint ROM as well as prevent progression to permanent joint contracture. Additionally, regular home-based stretching exercise performed by parents is a key factor in reducing joint stiffness. In conclusion, early rehabilitation therapy and faithful homebased exercise for patients with ScGVHD after HSCT is effective for improving joint ROM.
Notes
No potential conflict of interest relevant to this article was reported.
Conceptualization: Jung M, Sung IY, Ko EJ. Methodology: Jung M, Sung IY. Formal analysis: Jung M. Project administration: Sung IY. Visualization: Jung M. Writing - original draft: Jung M. Writing - review and editing: Sung IY. Approval of final manuscript: all authors.