Can Short-Term Constraint-Induced Movement Therapy Combined With Visual Biofeedback Training Improve Hemiplegic Upper Limb Function of Subacute Stroke Patients?
Article information
Abstract
Objective
To Investigate the synergic effects of short-term constraint-induced movement therapy (CIMT) and visual biofeedback training (VBT) in subacute stroke patients.
Methods
Thirty-two subacute stroke patients were enrolled and randomly assigned to one of three groups: short-term CIMT with VBT, VBT only, and control groups. We applied CIMT for an hour daily during VBT instead of the ordinary restraint time, referred to as 'short-term' CIMT. Short-term CIMT with VBT group received simultaneous VBT with CIMT, whereas the VBT the only group received VBT without CIMT for an hour a day for 2 weeks. The control group received conventional occupational therapy (OT) alone. Patients underwent the Purdue Pegboard Test, the JAMAR grip strength test, the Wolf Motor Function Test, the Fugl-Meyer Assessment (upper extremity), Motricity index and the Korean version of Modified Barthel Index test to evaluate motor functions of the hemiplegic upper limb at baseline, post-treatment, and 2 weeks after treatment.
Results
No significant differences were observed between short-term CIMT with VBT and VBT only groups. Both groups showed significantly higher scores compared to the control group in the WMFT and FMA tests. However, the short-term CIMT with VBT group showed significant improvement (p<0.05) compared with the control group in both grasp and pad pinch at post-treatment and 2 weeks after treatment while the VBT only group did not.
Conclusion
Short-term CIMT with VBT group did not show significant improvement of hemiplegic upper limb function of subacute stroke patients, compared to VBT only group. Larger sample sizes and different restraint times would be needed to clarify the effect.
INTRODUCTION
Most stroke survivors have upper limb motor impairments, along with difficulties in performing activities of daily living [1]. Currently, there are several known intervention treatments for functional recovery of the upper limb after stroke.
Constraint-induced movement therapy (CIMT) has been shown to enhance hemiplegic upper limb functions at both early and late stages of post-stroke [2]. The test was developed by Taub et al. [3] to improve the function of the affected upper limb by limiting the motion of the intact upper limb and induce affected upper limb movement [45]. The original CIMT program consisted of 2 weeks of restraining the unaffected upper limb for 90% of waking hours combined with forced use of the affected upper limb for approximately 6 hours per day during task-oriented activities. However, Page et al. [6] reported that 68% of 208 stroke patients said that they were disinterested in participating in CIMT. One domestic research study showed that 12 out of 46 patients dropped out when they participated in CIMT lasting for 14 hours daily for 2 weeks. The most common reason for dropping out in this study was the lack of participation in training time [7]. Therefore, in a clinical setting, various modified CIMT methods have been developed to improve participation rates.
Recently visual biofeedback training (VBT) has been studied and introduced as a therapeutic option because VBT might improve motor performance by effectively tuning the control structure [8]. Also, Kim et al. [9] reported a significant effect of spatial target reaching training based on visual biofeedback of the upper limb function in hemiplegic subjects. In their previous article, VBT group showed more significant improvement than the control group in the Wolf Motor Function Test (WMFT) and the Fugl-Meyer Assessment (FMA).
Several other studies have also been developed that recognize the effect of CIMT combined with other treatments [101112]. In these trials, unaffected upper limbs were restrained for several hours daily, even when participants were not taking other combined therapies. However, it is not easy to apply restraint for more than 5 to 6 hours daily in a clinical setting and longer restraint times can compromise a patient's therapeutic compliance. To overcome these limitations, it is necessary to find out whether there is any modified therapies have any effects such as a reduced restraint time in CIMT during combined therapy.
In this study, we applied a new CIMT protocol in a clinical setting, while maintaining the existing concept of CIMT. Both CIMT and VBT were performed simultaneously for 1 hour daily for 2 weeks. CMT is hereafter referred to as 'short-term' CIMT. We examined the effects of short-term CIMT combined with VBT on gross and fine motor functions and daily functions in patients with subacute hemiplegic strokes. We hypothesized that study participant who received short-term CIMT with VBT would demonstrate more improved outcomes than patients who received VBT alone.
MATERIALS AND METHODS
Participants
A total of 32 patients were enrolled in this study. Patients were recruited at the Soonchunhyang University Bucheon Hospital between April 2014 and December 2015. Inclusion criteria were as follows: (1) patients who were diagnosed with hemiparesis due to stroke (onset time of fewer than 3 months) and had no previous history of strokes; (2) patients who could perform an active extension of the affected wrist and more than 2 fingers at an angle >10° and an active abduction of the affected thumb at an angle >10°; (3) Korean version of the Mini-Mental State Examination score of 24 or higher; (4) patients who received care by guardians or caregivers; and (5) patients who could maintain a stable sitting position for more than 30 minutes. The exclusion criteria were as follows: (1) the spasticity of Modified Ashworth Scale (MAS) II or higher; (2) patients with limited upper limb exercises due to shoulder hand syndrome, secondary adhesive capsulitis, etc.; and (3) patients with visual problems.
They were then randomly assigned to three groups: short-term CIMT with VBT group (n=11), VBT only group (n=11), and control group (n=10). One participant of short-term CIMT with VBT group showed recurring cerebral infarction on the third day of participation and was transferred to the Department of Neurology. Another participant in the VBT only group had pneumonia on the fifth day of participation and was transferred to the Pulmonology Department. There was no further follow-up of these 2 patients, and they were excluded from the statistical analysis. In total, 30 patients were analyzed (Fig. 1). All patients were informed of the procedures and objectives of this study. The study protocol was approved by the Institutional Review Board (No. SCHBC2013-02-014-005).
Treatment methods
All three groups received conventional occupational therapy for one hour daily for 2 weeks without CIMT. Conventional occupational therapy consisted of fine motor exercises, upper-limb strengthening exercises, range of motion (ROM) exercise and training in the activities of daily living. The short-term CIMT with VBT group received visual biofeedback training with CIMT for 1 hour daily for 2 weeks. During the training, patients wore an orthosis specifically designed to limit the motion of the unaffected hand and wrist. The VBT only group received VBT without CIMT for 1 hour daily for 2 weeks. The control group received only the conventional occupational therapy.
E-LINK (Biometrics Ltd., Gwent, UK) was used for the VBT. The E-LINK program used a device connected to the computer. The device performs by connecting to the dynamometer and pinchmeter. Patients sat in the chair and looked at the computer monitor by holding the dynamometer or pinchmeter with their hemiplegic hand. Patients could flex their wrists, extend their limbs with dynamometers or could perform tip pinches and lateral pinch grips using the pinchmeter. Moreover, they could practice flexing their fingers by using disc grips (Fig. 2).

Four possible motions in E-LINK program. (A) Disc grip. (B) Tip pinch. (C) Lateral pinch. (D) Wrist flexion and extension.
There are many games, such as 'Bricks,' 'Maze,' 'catch balls,' 'drop balls,' 'tumble,' and 'find a space,' in the E-LINK program. Patients could select their preferred games. They were engaged in computer-generated games displayed on a video monitor. A start signal was provided to indicate the initiation of the game. Patients were required to gaze the target on the monitor. Then they were instructed to reach the target by holding the device connected to their computer. Patients were instructed to move the dyanamometer or pinchmeter in order to move the target on the monitor. Before the start of training, the dynamometer and pinchmeter were set to fit properly, and according to the patient's muscle strength and ROM, that is, individualized ROM was set as the target's maximum distance that appeared on the monitor. Maximal ROM, which patients could move, was allowed in training.
In addition to the game program, the patients also performed 'behavior simulation' as virtual reality training in the E-LINK program. This training included combing, spooning and drinking water. For example, the virtual person taking a spoon appeared on the monitor. To move the spoon, the patient had to move disc grip. Then the patients were prompted to try to get the spoon to the mouth by forearm pronation and supination (Fig. 3). These acts were repeated. The VBT included 30 minutes of game training and 30 minutes of 'behavior simulation' training. One session consisted of 5-minute training, followed by a 1-minute period of rest. Patients performed a total of 10 sessions per day. If ROM of the wrist and fingers increased, the ROM and resistance of the device were adjusted accordingly. Whenever patients in short-term CIMT with VBT group finished the first session, they received immediate feedback on their task performance followed by positive reinforcement of improvements (shaping element).
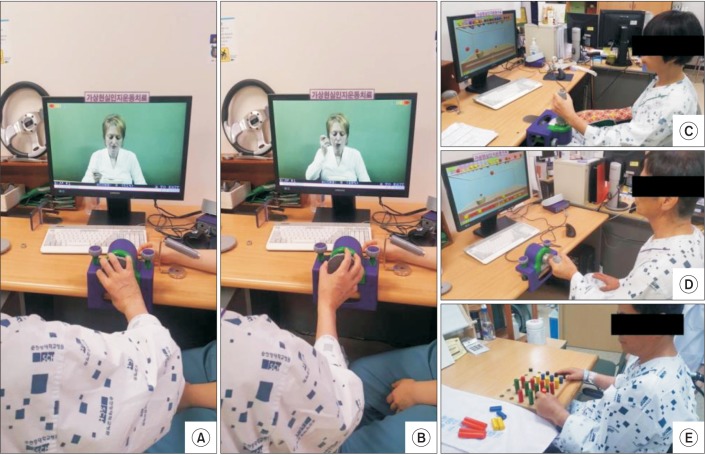
The patient with right hemiparesis received 'behavior simulation.' The patient held a disc grip by finger flexors. (A) The patient tried to put the spoon in the bowl by forearm pronation. (B) On the other hand, the patient was required to supinate his forearm for getting the spoon to the mouth. There were three patients with left hemiparesis. (C) One received short-term CIMT and VBT simultaneously. (D) Another patient received only VBT. (E) Both patients participated in the catch balls' game. The other patient received conventional occupational therapy. CIMT, constraint-induced movement therapy; VBT, visual biofeedback training.
The following tests were evaluated at baseline, post-treatment and at 2 weeks of follow-up for each group: Perdue Pegboard Test, JAMAR grip strength test, Wolf Motor Function Test, Fugl-Meyer Assessment (upper extremity), Motricity index and the Korean version of Modified Barthel Index.
Statistical analysis
SPSS ver. 14.0K for Windows (SPSS Inc., Chicago, IL, USA) and R ver. 3.1.3 (The R Foundation for Statistical Computing, Vienna, Austria) were used for statistical analyses. Baseline characteristics of the study groups were summarized as count and percentage for categorical variables, and as the mean and standard deviation (SD) for continuous variables. Group comparisons were used by the Fisher exact test for qualitative variables and the Kruskal-Wallis test for quantitative variables.
Friedman two-way analysis of variance by ranks was used to evaluate any significant difference among short-term CIMT with VBT, VBT only, and the control group at baseline, post-treatment and 2 weeks after treatment. For each measurement, time, group, and interaction effect were tested. In the case of the significant interaction effect, the Kruskal-Wallis test was applied to evaluate the difference among the three groups at each time point. We also used the Bonferroni method for post-hoc analysis and set a level of statistical significance at p<0.017. In addition, we used the Kruskal-Wallis test to evaluate the amounts of change among three groups compared to the baseline at each time point. When significant, the Mann-Whitney U-test was performed. A p-value of <0.05 was considered statistically significant for the Kruskal-Wallis test, and a p-value <0.017 was considered significant for the Mann-Whitney U-test.
RESULTS
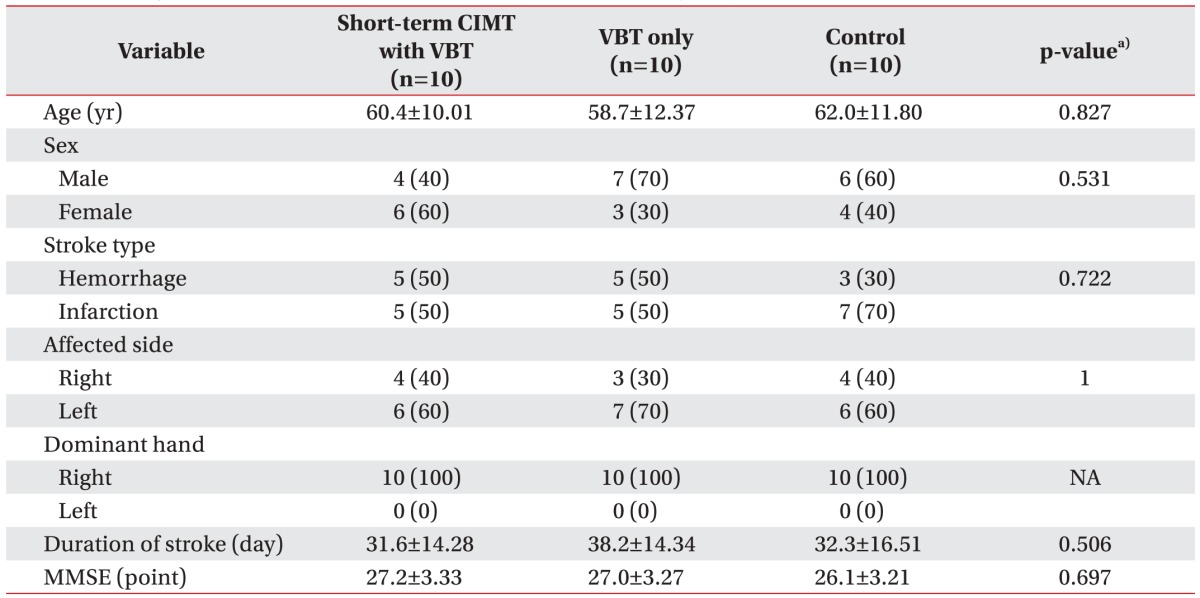
The 32 patients enrolled in this study were randomized and divided into three groups. As mentioned above, 2 patients were not followed up due to a medical problem. A total 30 patients were analyzed, with each group assigned ten subjects. The distribution at baseline showed no statistically significant differences (Table 1).
For all 9 measured variables, significant improvements were observed from the pre-treatment to 2 weeks after treatment. The exception was the grasp variable, which showed the tendency of group effect (p=0.074), although it was not statistically significant. On three occasions (i.e., before-treatment, post-treatment and 2 weeks after treatment) the mean grasp value was the highest for the short-term CIMT with VBT group and lowest in the control group.
Interaction effects between time and the group were significant in two variables with pad pinch (p<0.05) and FMA (p<0.05). But these variables did not show statistical significance using the post-hoc analysis. However, the short-term CIMT with VBT group showed lower FMA scores than other groups at the pre-treatment stage, but they were reversed at both post-treatment and 2 weeks after treatment (Table 2).
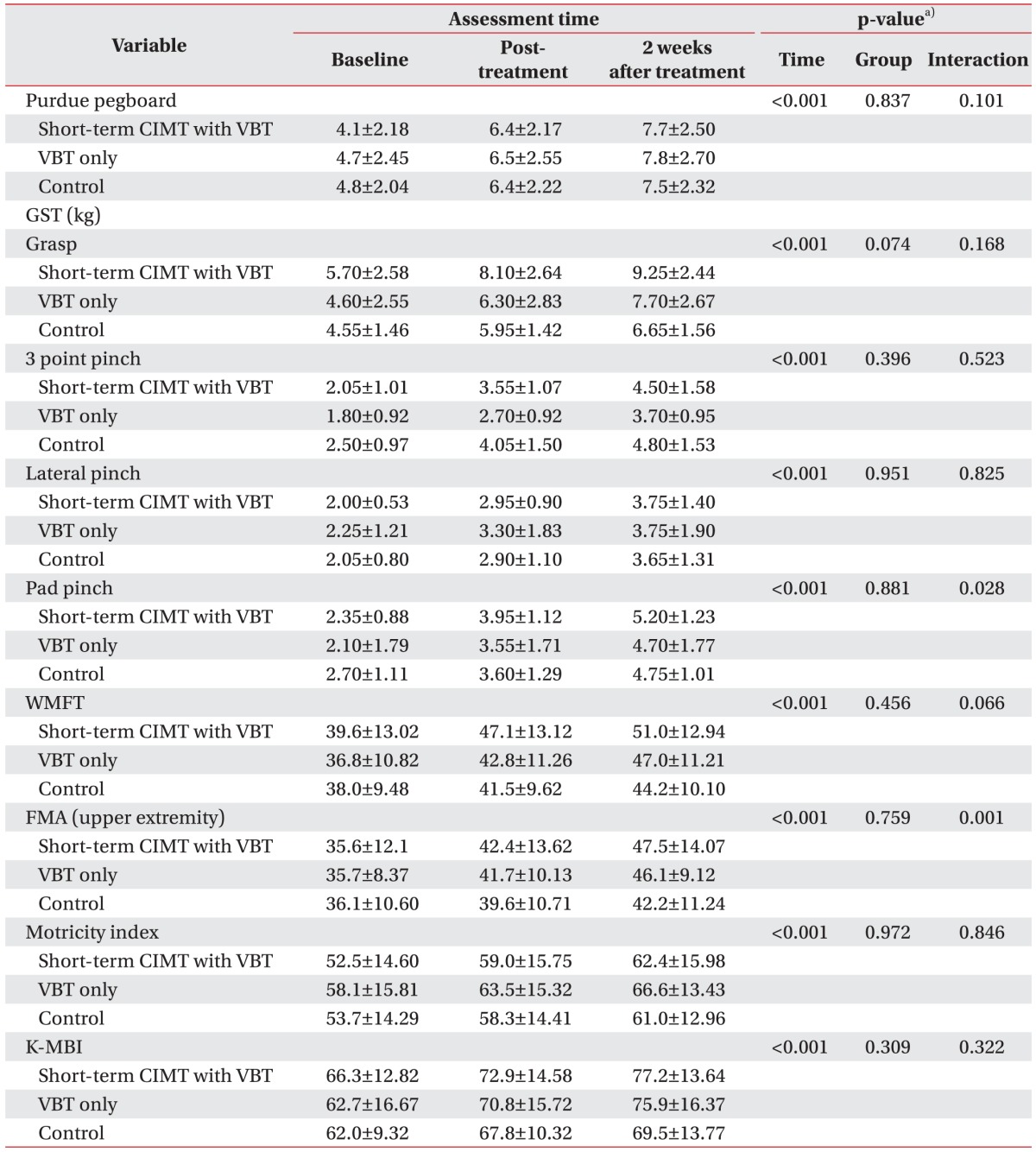
Comparison assessments at baseline, after treatment, and 2 weeks after treatment in the three groups
We could not obtain significant differences among them when using the Friedman test by taking time and group into consideration. Thus, we observed the amounts of change among three groups in comparison to the baseline at each time point. In the results of the Kruskal-Wallis test, grasp at post-treatment was significantly different (p<0.05) and the short-term CIMT with VBT group had significantly higher grasp score than the control group, while the VBT only group did not show statistically significant improvement in comparison to the control group. However, there was no significant difference at 2 weeks after treatment. The short-term CIMT with VBT group showed a significant improvement as opposed to the control group in pad pinch at both post-treatment (p<0.05) and 2 weeks after treatment (p<0.05). But, the VBT only group showed no significant difference in comparison to the control group. In WMFT and FMA, short-term CIMT with VBT and VBT only group showed significantly higher scores at post-treatment and 2 weeks after treatment (p<0.05) when compared to the control group. All variables, which showed significant improvement by the Kruskal-Wallis test, did show statistical significance using the post-hoc analysis. But there were no significant differences between short-term CIMT with VBT and VBT only groups (Table 3, Fig. 4). No adverse event was reported in short-term CIMT with VBT and VBT only groups. None of the patients complained about the treatment during the study period. All patients in both groups reported VBT was well tolerated and enjoyable.
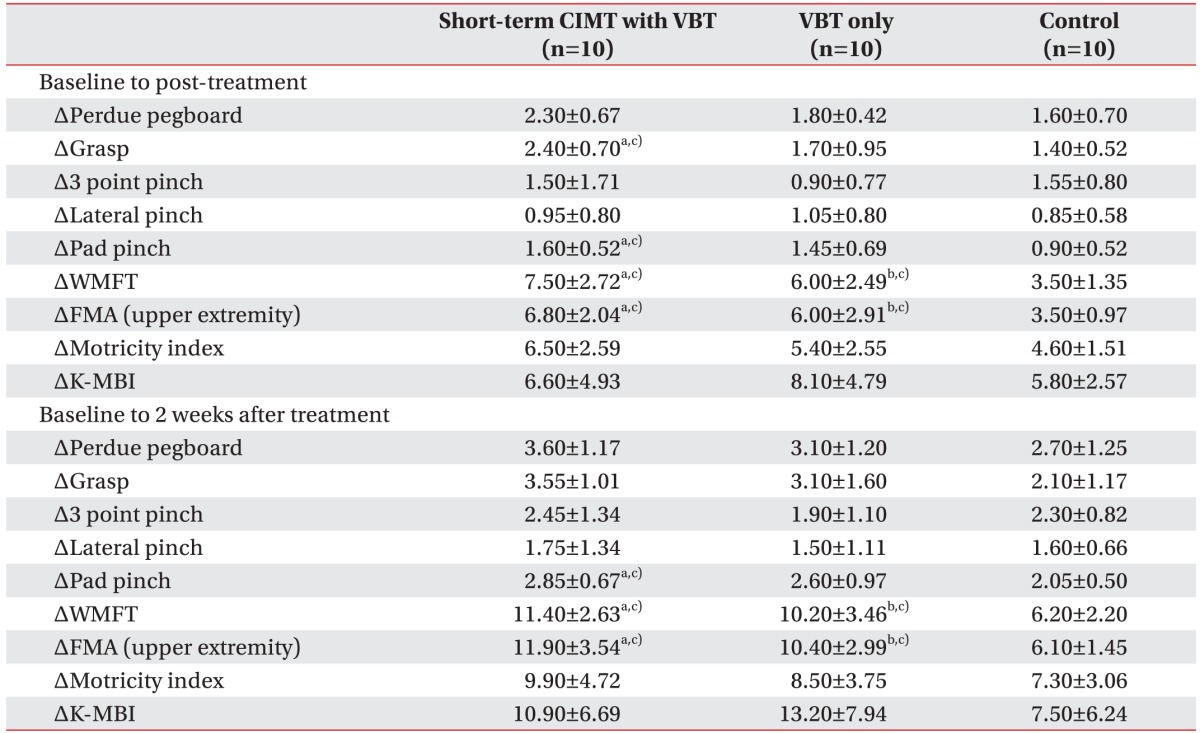
Comparison of improvement of clinical parameters at post-treatment and 2 weeks after treatment in each group
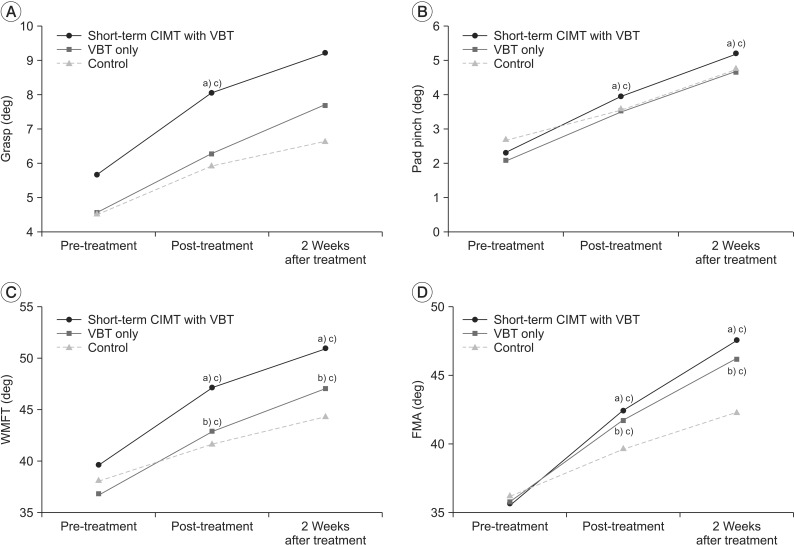
This figure shows sequential changes in clinical parameters at post-treatment and 2 weeks after treatment in each group. Changes in grasp (A), pad pinch (B), WMFT (C), and FMA (upper extremity) (D). CIMT, constraint-induced movement therapy; VBT, visual biofeedback training; WMFT, Wolf Motor Function Test; FMA, Fugl-Meyer Assessment. a)p<0.05 (short-term CIMT with VBT group vs. control group), b)p<0.05 (VBT only group vs. control group), c)p<0.017 by the Mann-Whitney U test for post-hoc analysis.
DISCUSSION
A considerable number of patients experience disabilities following strokes [13]. More than half of stroke patients would experience difficulties in performing their daily activities, in particular, due to impairment of the upper limbs. This continues for a few months to several years after a stroke [14]. Although in most cases the function of the upper limb may recover within 6 months, complete recovery occurs only in about 12% of the patients after stroke [1]. In this study, we examined the effects of the short-term CIMT with VBT on gross and fine-motor functions and daily function in subacute hemiplegic stroke patients.
Each of the three groups showed statistically significant changes after treatment in the function of the hemiplegic upper limb. These changes persisted for 2 weeks after treatment. However, only the grasp variable showed a tendency of group effect, which was not significant. Though, the short-term CIMT with VBT and VBT only groups showed statistically significant improvements as opposed to the control group in the amounts of change of some variable sat post-treatment and 2 weeks after treatment from the baseline. These groups, in particular, had significant improvements in WMFT and FMA in comparison to the control group. Although these results were consistent with those observed in a previous study [9], our study demonstrates that significant improvements were maintained even at 2 weeks after treatment (VBT).
VBT included virtual reality training in our study. Participants practiced similar motions during virtual reality training, as discussed by Holden [15]. Similar to this study, we also observed a significant improvement in the upper limb function without adverse effects. In another study, Yin et al. [16] evaluated virtual reality training in the context of functional recovery of the upper limb after stroke. All patients reported that the training was enjoyable and helped the recovery of their hemiplegic upper limb. Our study further strengthens these observations by demonstrating that the virtual reality training is a feasible and enjoyable method as a stroke rehabilitation strategy.
Several researchers have evaluated the effects of CIMT combined with other treatments. Yoon et al. [11] performed CIMT combined with the mirror therapy for hemiplegic patients after stroke. Combination group showed more improvement than CIMT only group in the fine motor functions of the hemiplegic upper limb. Another study performing CIMT with EMG biofeedback training for hemiplegic stroke patients [12], also showed the efficacy of treatment in enhancing the motor skills of the hemiplegic upper limb. This effect was maintained until 2 weeks after treatment. In these studies, it is to be noted that the CIMT and other treatments were not performed simultaneously. However, in our study we combined CIMT with other treatments (VBT) and performed them simultaneously to reduce the restraint time in CIMT for improving patient compliance. Blanton et al. [17] emphasized that the integrated approaches with CIMT such as robotics, virtual environments, mental imagery, etc., need to be explored in future studies. The aim of our study was to examine the combined effect of VBT with CIMT, which is in accordance with the future directions for research.
Therapeutic effects of the short-term CIMT were also investigated in our study. Woldag et al. [18] had reported no significant improvement in the recovery of hemiplegic upper limb function, when the hemiplegic stroke patients received repetitive training of their hemiplegic upper limb for 10 minutes each, twice daily for 2 weeks. However, in another study, they reported that repetitive training with shaping was beneficial for motor improvement without its relevant transfer to functional improvement [19]. In their study, however, they did not restrain the unaffected upper limb during the training. The restraint component of CIMT has not been fully established [20]. Morris et al. [5] suggested that intensive training was more important than restraint. Intensive training for 90 minutes daily for 3 weeks using 'shaping' without restraining the unaffected limb showed significant functional improvement compared with the baseline [21]. Another study showed that restraint alone, using the mitten every other day for 2 week period for another 3 months (in total 21 days), did not enhance the therapeutic effect following CIMT [22]. Moreover, it was difficult to measure real restraint time precisely in a clinical setting [23].
However, interestingly, Treger et al. [24] evaluated patterns of hemispheric activation in post-stroke patients during motor tasks with and without arm restriction. They used transcranial Doppler sonography for measuring mean blood flow velocity to the middle cerebral artery. Significant elevation in the mean velocity of blood flow to the damaged middle cerebral artery was recorded immediately in post-stroke patients with restrained unaffected hand. In other words, restraint alone increased the velocity of blood flow to the damaged area while performing the task with affected limb.
However, these results were not known as the direct effect of the upper limb function recovery. Further, in most modified CIMT studies, participants are typically requested to restrain the unaffected upper limb for up to 5–6 hours daily and to have intensive training time from 30 minutes to 3 hours. When training time was 30 minutes to 1 hour, the total training period was extended to 10 weeks [25]. However, the 10 weeks treatment period is too long duration for the hospitalized patients. Besides, Pedlow et al. [26] investigated the compliance of CIMT 1-to-1 therapy during a 2–3 week period. It was noted that about 53% of therapist reported patients would comply with CIMT for a maximum of 1.5 hours per day. In other words, previous modified CIMT interventions still posed many practical difficulties. Considering this, we reduced the training period to 2 weeks to meet the clinical application and investigated the benefit of short-term CIMT for hemiplegic upper limb recovery based on previous results [24]. In order to eliminate patient's complaint due to restraining time of the unaffected upper limb, such as discomfort, pain and lack of gait training time, [7] no additional restraining time was given, except during the combined training session in this study. As a result, there were no patients who refused CIMT and there were no complaints about the treatment method. Positive effects of the short-term CIMT were observed in our study.
However, short-term CIMT with VBT group did not show significant functional improvements, compared to VBT only group. Short-term CIMT with VBT group showed significantly higher grasp and pad pinch score than the control group, while the VBT only group did not. CIMT was also developed to overcome 'learned nonuse' phenomenon of the hemiplegic upper limb [3]. So, restraining unaffected limb was encouraged while performing daily activities in the real world. From our study, it can be supposed that restrained time was too short to overcome learned nonuse completely. Burns et al. [27] reported that the use of a mitten in the unaffected upper limb for 9 hours per day for 2 weeks showed considerable improvement in the Action Research Arm Test (ARAT) score compared with the non-use of a mitten. Compared to our study, constraint time was longer. It was thought that the difference of constraint time might lead to the difference of functional improvements.
This study has several limitations. First, it is not advisable to generalize our results in subacute stroke patients with hemiplegic upper limb because of the small sample size analyzed in our study. Second, since we followed up patients for only 2 weeks after treatment, no long-term effects were evaluated. Third, we could not examine functional recovery in stroke patients with severe cognitive impairment or spasticity because we used the Mini-Mental Status Examination, MAS scale, and manual muscle test to screen the patients initially. Last, we did not investigate the correlation between functional recovery and cortical reorganization by using imaging study, such as magnetic resonance imaging (MRI). In this context, it is important to mention that a previous study has shown an increase in gray matter in the sensory and motor areas in bilateral hemispheres coincident with the improvement in hemiplegic upper limb function after CIMT [28]. But in this study, patients underwent constraining of the intact upper limb for almost 90% of waking hours. So, further studies are needed to confirm the minimal time needed to ensure the effectiveness of CIMT by measuring cortical reorganization with MRI in accordance with the restraint time.
In conclusion, this is the first study that examined whether or not 1 hour daily CIMT (short-term CIMT) instead of ordinary restraint time might be beneficial for the hemiplegic upper limb function in subacute stroke patients. Short-term CIMT with VBT group did not show significant improvement of hemiplegic upper limb function in comparison with VBT only group. However, our study found a possibility of the short-term CIMT for clinical use because of high compliance and no patient dropout rate throughout the intervention period. Furthermore, the short-term CIMT with VBT group showed significant improvement compared with the control group in both grasp, and pad pinch while the VBT only group did not. A further study with tolerable different restraint time and larger samples will be needed to clarify these results.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.