Optimal Needle Placement for Extensor Hallucis Longus Muscle: A Cadaveric Study
Article information
Abstract
Objective
To determine the midpoint (MD) of extensor hallucis longus muscle (EHL) and compare the accuracy of different needle electromyography (EMG) insertion techniques through cadaver dissection.
Methods
Thirty-eight limbs of 19 cadavers were dissected. The MD of EHL was marked at the middle of the musculotendinous junction and proximal origin of EHL. Three different needle insertion points of EHL were marked following three different textbooks: M1, 3 fingerbreadths above bimalleolar line (BML); M2, junction between the middle and lower third of tibia; M3, 15 cm proximal to the lower border of both malleoli. The distance from BML to MD (BML_MD), and the difference between 3 different points (M1–3) and MD were measured (designated D1, D2, and D3, respectively). The lower leg length (LL) was measured from BML to top of medial condyle of tibia.
Results
The median value of LL was 34.5 cm and BML_MD was 12.0 cm. The percentage of BML_MD to LL was 35.1%. D1, D2, and D3 were 7.0, 0.9, and 3.0 cm, respectively. D2 was the shortest, meaning needle placement following technique by Lee and DeLisa was closest to the actual midpoint of EHL.
Conclusion
The MD of EHL is approximately 12 cm above BML, and about distal 35% of lower leg length. Technique that recommends placing the needle at distal two-thirds of the lower leg (M2) is the most accurate method since the point was closest to muscle belly of EHL.
INTRODUCTION
The extensor hallucis longus muscle (EHL) arises from the middle half of the fibula and the adjacent interosseous membrane, and extends deeply between the tibialis anterior and the extensor digitorum longus muscle [1]. The fibers pass downward, and end in a tendon, which occupies the anterior border of the muscle in the lower one third of the leg and is inserted into the base of the distal phalanx of the great toe [2].
EHL is an important muscle in evaluation and diagnosis of deep peroneal nerve [34] or distal segment of L5, S1 roots lesions through electromyography (EMG). It is preferred over other foot intrinsic muscles with same innervations and myotome because foot intrinsic muscle have high false positive abnormality [5]. However, blind technique for needle placement had low accuracy in lower-limb muscles with mean percentage of insertions that penetrated the intended muscle of 57%, although success rate of EHL was 80% [6].
EHL needle insertion points for needle EMG vary according to textbooks [789]. Perotto et al. [7] typically used the examiner's fingerbreadth as a measure, and suggested to insert the needle at 3 fingerbreadths above the bimalleolar line of the ankle just lateral to the crest of the tibia. Lee and DeLisa [8] recommended inserting the needle at the junction between the middle and lower third of the tibia and at the space between the tendons of tibialis anterior and extensor digitorum longus. Chu-Andrews and Johnson [9] preferred to insert the needle 15 cm proximal to the bimalleolar line between the tendons of tibialis anterior and extensor digitorum longus. The diversity in methods from three commonly referred textbooks in Korea is suggestive of the difficulty in accurate EHL localization.
Therefore, this study was designed to firstly determine the midpoint (MD) of EHL with cadaver dissection and to decide the most accurate method by comparing the distance difference from actual MD of EHL.
MATERIALS AND METHODS
Thirty-eight limbs of 19 embalmed cadavers (10 men, 9 women) were dissected. Skin and subcutaneous tissue were dissected first. Then, needle insertion was conducted according to three different commonly referred methods [789]: 3 fingerbreadths above bimalleolar line just lateral to the crest of the tibia (M1); the junction between the middle and lower third of the tibia and at the space between the tendons of tibialis anterior and extensor digitorum longus (M2); 15 cm proximal to bimalleolar line between the tendons of tibialis anterior and extensor digitorum longus (M3). After marking these three points according to different textbook (M1–3), superficial muscles of anterior compartment of lower legs were removed to expose entire EHL. Bimalleolar line (BML) was drawn between the inferior tip of medial and lateral malleolus. The most proximal part of EHL, where the muscle first starts from fibula was marked as proximal origin (PO) and the most distal part of the muscle attached to fibula was marked as distal origin (DO). The most distal part where muscle portion remained and changed to tendon portion was marked as musculotendinous junction (MT).
As shown in Fig. 1, the distance from BML to the proximal and distal origin of EHL on the fibula and MT were measured (BML_PO, BML_DO, and BML_MT, respectively). The distance was measured parallel to the axis of tibia. The midpoint of EHL (MD) was marked at the middle point between the proximal origin and musculotendinous junction of EHL. The distance between BML and MD (BML_MD), and the lower leg length (LL), defined as the distance between BML and the top of medial condyle of the tibia were measured. The ratio of BML_MD to LL was also calculated in percentage. The distance was measured in proximal direction from MT or MD. Thus, the distance was recorded in minus values if the measuring points were located distal to MT or MD.

Needle insertion sites according to three different commonly referred methods: M1, 3 fingerbreadths above the bimalleolar line; M2, junction between the middle and lower third of tibia; M3, 15 cm proximal to the lower border of both malleoli. Bimalleolar line was drawn between lower borders of both malleoli. The distance from bimalleolar line to proximal (BML_PO) and distal origin (BML_DO) of extensor hallucis longus (EHL) was calculated. Musculotendinous junction (MT) and midpoint (MD) of EHL was also marked.
The Distances From Bml To Three Different Needle Insertion Points Were Measured And Named Bml_m1, Bml_m2, And Bml_m3, Respectively (Fig. 1). In Order To Assess And Compare The Accuracy Of Needle Placement, The Difference In Distance Between Md And M1, M2, And M3 Was Calculated, I.E., D1, D2, And D3, Respectively.
Nonparametric statistical test was used since Shapiro-Wilk test of the data did not show normal distribution, and due to small number of cadavers. Median and range (minimum–maximum) of each parameter were recorded. Side to side comparison of each parameter was performed with Wilcoxon signed-rank test using SPSS software ver. 20.0 (IBM, Armonk, NY, USA).
RESULTS
Median distance from BML to musculotendinous junction (BML_MT) was –1.0 cm; the median distance from BML to distal origin on the fibula (BML_DO) was 7.3 cm; to proximal origin (BML_PO), 23.8 cm. The median distance from BML to midpoint of EHL (ML_MD) was 12.0 cm and the median lower leg length was 34.5 cm. The percentage of BML_MD to total lower leg length was 35.1%, which means midpoint of EHL was located in distal 35% of total lower leg length. The median distance difference between midpoint and each needle insertion points (D1, D2, and D3) were 7.0 cm (4.0–9.0), 0.9 cm (0.0–4.1), and 3.0 cm (0.5–5.5), respectively (Table 1). Minus values in BML_MT indicated that the musculotendinous junction started distal to bimalleolar line.
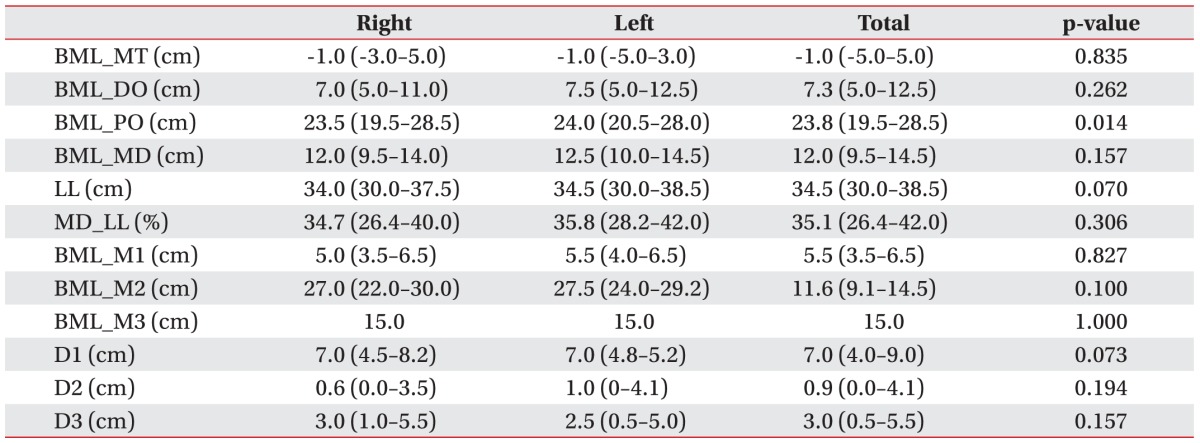
Anatomical parameters of extensor hallucis longus and distance from points designated by three different methods
There were no statistically significant differences of anatomical parameters except BML_PO between right and left sides.
DISCUSSION
EHL is a frequent target muscle for botulinum toxin injection in patients with lower extremity dystonia and spasticity and a sample muscle for diagnostic electromyography. Yet, due to its deep location and uneven muscle fibers, its approach for needle EMG is challenging. Accordingly, different textbooks for needle EMG suggest different needle insertion points for EHL [789]. The various EHL needle insertion techniques from textbooks imply the difficulty of blind localization of EHL. Several studies have compared the accuracy rates of blind needle placement and confirmed mishitting rates of EHL during blind needle insertion [10].
In 2003, a cadaver study investigated the accuracy of lower-limb techniques described in the texts by Perotto et al. and Geiringer [6]. In 2007, another cadaver study investigated the accuracy of the same techniques in both upper and lower limbs [11]. Both of these studies quantified the accuracy through actually inserting the wired needle to a cadaver and checking the location of the needle tip through dissection. However, these studies have limitations since the results can be influenced by disparity of technical experience among different physicians and by denatured state of the skin and muscle due to chemical embalmment. In contrast, our study focused solely on EHL muscle with larger number of cadavers, and compared the accuracy of the techniques through comparing each target location to actual muscle belly of EHL through cadaver dissection. To the best of our knowledge, it is the first study to compare three different needle electrode placement techniques through cadaver dissection.
Inaccurate needle insertion increases the possibility of hitting an incorrect muscle, tendon, or nerve [6]. If the needle is inserted too superficially and too proximally, it might end in the tibialis anterior muscle. If inserted too laterally or distally, it might hit the peroneus tertius muscle, and even end in tendon portion [7]. Because the pattern of electrodiagnostic abnormality is critical in making the correct diagnosis, needle EMG needs to be accurate in sampling the selected muscles [11]. Incorrect needle placement compromises the diagnostic utility of the procedure leading to misdiagnosis [6]. In addition, inaccurate placement of botulinum toxin can result in suboptimal efficacy or undesired weakness in unaffected muscles [10].
In order to improve the accuracy of needle insertion of EHL, advance imaging with ultrasonography or MRI might be helpful. However, these imaging studies are time consuming and costly, hence, the physicians often prefer blind needle EMG, with the exception of patients who are unconscious or unable to recruit muscles in isolation. Therefore, in order to maximize successful blind needle insertion of EHL, it is important to accurately localize the muscle belly of EHL by following the best method that is most accurate.
Recently, the clinical importance of EHL has increased with the frequent use of botulinum toxin therapy in foot pathology. Patients with foot dystonia, problematic upgoing toe (EHL hyperextension), and spasticity of many other disorders such as traumatic brain injury, spinal cord injury, multiple sclerosis and others [31213] are treated through chemodenervation, either by botulinum toxin or alcohol, in order to decrease abnormal EHL hyperactivity. In these cases, it is very important to localize the motor point of EHL.
Among cadaveric studies on motor point of EHL, Elgafy et al. [14] reported that a high-risk zone of iatrogenic lesions of the innervation of the EHL was between 5.9+1.7 cm and 10.9+1.7 cm from the most distal point of the fibular head. Other cadaveric study of 31 limbs demonstrated that 24 limbs had one motor branch and 5 limbs had two motor branches to EHL. The median distance between the origin of the first branch for EHL and the most prominent point of the fibular head was 8.8 cm (range, 0–13.7 cm), and median distance between the origin of the second branch for EHL and the most prominent point of the fibular head, 12.5 cm (range, 9–14.2 cm), which was not proportional to the length of the leg [3]. These findings showed that the motor point of EHL might be widely distributed along the muscle belly. Although the majority of skeletal muscles possess one motor point region typically located halfway between the muscle's origin and insertion [15], some muscles could have more than two motor points. In EHL, which has long tendon portion, it is practical to locate the proximal and distal end of the muscle portion and bisect it in order to find the most likely motor point.
As shown in Table 1, the MD of EHL, which is considered ideal EHL needle insertion point in this study, was about 12 cm above the bimalleolar line, located at distal 35% of total lower leg length. Among three needle insertion points (M1, M2, and M3) using three different techniques, M2 was closest to MD with median distance difference (D2) of 0.9 cm. Therefore, second method by Lee and DeLisa [8], which used the proportion of the lower leg length as measurement, is the most accurate technique. This is a reasonable result considering the limitations of other two techniques. The first method by Perotto et al. [7] is not precise due to disparity of examiner's finger width and is too distal with only small portion of the muscle evaluated. The third method by Chu-Andrews and Johnson [9], which used an absolute fixed distance (15 cm), has limitation since all individuals have different lower leg lengths, which makes it not widely applicable, especially to children. The side to side difference was statistically significant in only BML_PO. This is probably due to some of the cadavers with leg length difference of maximal 2.5 cm.
There were several limitations in our study. First of all, the actual motor point was not evaluated in this study. Instead of detecting motor point through identifying actual EHL muscle penetration of the deep peroneal nerve, this study designated the midpoint of the muscle portion of EHL as most likely motor point according to the textbook [15]. Secondly, this study only concentrated in the distance of needle insertion point from the bimalleolar line neglecting the depth of the needle insertion. Accurate needle insertion includes appropriate depth, especially in deep muscles such as EHL. However, this study did not consider depth because accurate depth cannot be evaluated in embalmed cadavers with muscle and skin shrinkage and chemical transformation. Lastly, location of neurovascular bundle and nearby covering muscles was not considered in the needle insertion point. Since the objective of this study was to determine which method was closest to the muscle midpoint, other risk factors such as anatomical proximity to the neurovascular bundle were not evaluated. Moreover, due to chemically embalmed state of the cadaver, the covering muscles were necessarily removed in advance. If these limitations were supplemented, the results may have been more precise and accurate.
In conclusion, the muscle belly of EHL is located at about 12 cm above bimalleolar line and, in proportion, at about distal 35% of total lower leg length. Considering different lower leg length among patients, it is preferable to use proportion as measurement. Therefore, the approximately distal third part of the lower leg is practical for accurate needle insertion of EHL. Among three different methods, M2 was the closest to actual midpoint of the muscle, which indicates the most accuracy.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
