ICF Based Comprehensive Evaluation for Post-Acute Spinal Cord Injury
Article information
Abstract
Objective
To evaluate the feasibility of the ICF for initial comprehensive evaluation of early post-acute spinal cord injury.
Method
A comprehensive evaluation of 62 early post-acute spinal cord injury (SCI) patients was conducted by rehabilitation team members, such as physicians, physical therapists, occupational therapists, nutritionists, medical social-workers, and nurses. They recorded each of their evaluation according to the ICF first level classification. The contents of the comprehensive evaluation were linked to the ICF second level categories, retrospectively. The linked codes were analyzed descriptively and were also compared with the brief ICF core set for early post-acute SCI.
Results
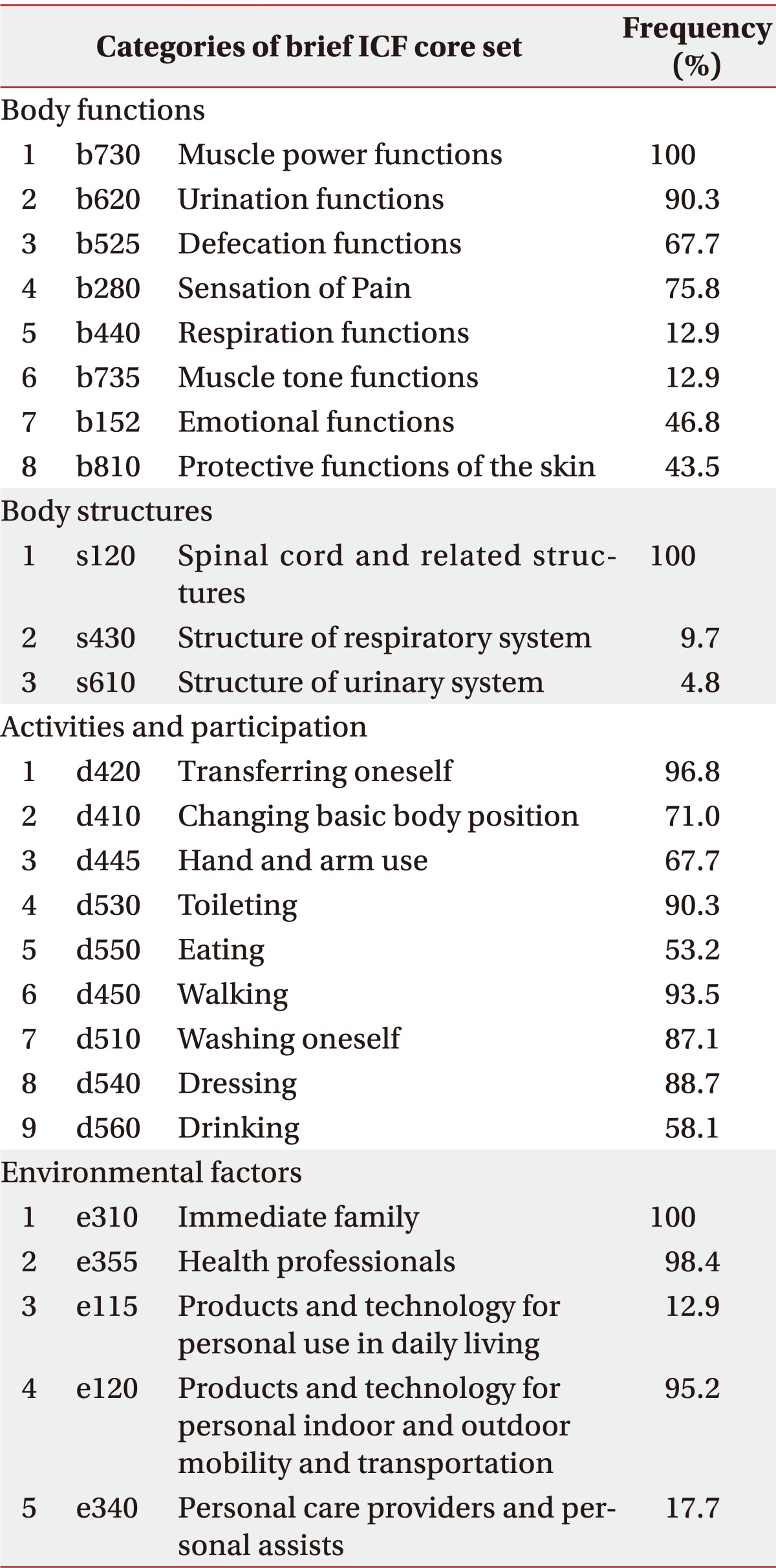
In the evaluation of early post-acute SCI patients based on the ICF first level categories, 19 items from the body functions domain, such as muscle power functions (b730) and urination functions (b620), 15 items from the body structures domain, including spinal cord and related structures (s120), 11 items from the activities and participation domain, such as transferring oneself (d420) and walking (d450), and 9 items from the environmental factors domain, e.g., health professionals (e355), were linked to the ICF second level categories. In total, 82.4% of all contents were linked to the brief ICF core set. Prognosis insight, a personal factor not linkable to an ICF code, was mentioned in 29.0% of all patients.
Conclusion
First level ICF categories can provide a structural base for a comprehensive evaluation in early post-acute spinal cord injury. However, frequently linked items, including the brief core set, as well as personal factors should be considered via a checklist in order to prevent the omission of significant contents.
INTRODUCTION
Spinal cord injury (SCI) results in the impairment of several body functions and therefore, numerous changes occur in the daily lives of SCI patients. When acute SCI occurs, the patient is transported to the emergency room and undergoes operation, if necessary. After the vital sign and the patient status are stabilized, the rehabilitation process begins. In traumatic SCI, adequate timing of medical treatment and rehabilitation is essential for the recovery of functioning. It is known that functioning prognosis is better if the time lapse from the injury to the rehabilitation department admission is shorter.1 The concept of "post-acute rehabilitation" can be understood as the rehabilitation process being initiated as soon as possible after acute medical management.2 In the rehabilitation of SCI patients, specific therapies, such as physical therapy, occupational therapy, and respiratory rehabilitation therapies should be carried out simultaneously, and medical treatments for symptoms including orthostatic hypotension, pain, and spasticity, are also required. Considerations on socioeconomic aspects, such as occupation, are also important because the age group of SCI patients are younger compared to the other disease categories, such as stroke. As described above, rehabilitation of SCI patients requires focusing on various aspects. Therefore, a comprehensive evaluation on the patient's medical, functional, and social status is necessary before planning the rehabilitation therapy and goals.3 In the comprehensive evaluation of SCI, the problem list oriented approach is known to be more useful than the individual approach by each rehabilitation team member.4
In 2010, Kirchberger and colleagues2,5 suggested the International Classification of Functioning, Disability and Health (ICF) core sets for acute and chronic spinal cord injury. ICF core set is a list of important items regarding the evaluation of functioning and disability in a specific disease entity, by gathering opinions and consensus from experts of that specific disease. Specifically, it is a collection of relevant factors involved in common functional impairments and environmental factors that must be taken into consideration. The ICF core set is established for many disease categories because the whole ICF classification system is very extensive.6-8
Rauch et al.9 suggested that the ICF core set can be used to describe the patient's functioning status comprehensively and a more efficient approach can be made for rehabilitation by application of the ICF core set. They also conducted and analyzed the comprehensive evaluation of one spinal cord injury person and suggested a conceptual framework of the comprehensive evaluation.10 But to our knowledge, the practical proposal on the usage of ICF in the clinical rehabilitation field has not been reported so far. In our hospital, we have been conducting a comprehensive evaluation for SCI patients for 3 years from 2008 by the problem list oriented method based on the ICF 1st level classification. In this study, we analyzed the comprehensive evaluation records and coded the contents according to the ICF 2nd level classification. We aimed to investigate the utility of the ICF in the problem list oriented comprehensive evaluation of post-acute SCI patients and suggest a specific practical method of evaluation.
MATERIALS AND METHODS
In our hospital, when a patient is admitted to the rehabilitation unit, comprehensive evaluation is carried out within 1-2 weeks. The patient is evaluated in various aspects, and then, the short-term and long-term rehabilitation goals are set. Every rehabilitation team member involved with the patient in any way participates in the comprehensive evaluation meeting. The rehabilitation team consists of physiatrists, physical therapists, occupational therapists, nurses, nutritionists, medical socialworkers, etc. Prior to the year 2008, the comprehensive evaluation was conducted from the viewpoint of each rehabilitation team member. However, from 2008 and on, the evaluation was accomplished within a framework of the ICF 1st level classification (Fig. 1). The evaluation form was created according to the problem list oriented method based on the ICF 1st level classification. Each rehabilitation team member filled out the blanks for each category with the contents they have assessed and evaluated. Then, all of the members joined the meeting and participated in active discussions about the evaluation contents.
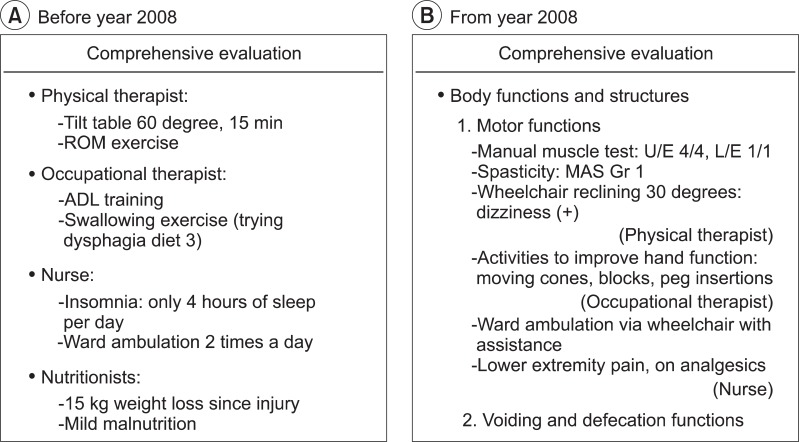
Templates for the comprehensive evaluation of early post-acute SCI. (A) Each member of the rehabilitation team fills out the patient's status in their point of view, independently. (B) The template is divided by major ICF first level categories, and for each category, members of the rehabilitation team fill the form according to their view.
Subjects
We retrospectively reviewed 90 reports of the comprehensive evaluation that were performed from February, 2008 to June, 2011. Sixty-two cases, which met the criteria for post-acute SCI, were selected for analysis: 1) spinal cord injury confirmed by spine magnetic resonance imaging (MRI), and 2) initial comprehensive evaluation performed within 2 weeks after admission to rehabilitation unit, following acute management in neurosurgery or orthopedic surgery department. Five cases were excluded because they were re-evaluation reports, and 23 cases were excluded because initial evaluation was done after 2 weeks from admission, which were not suitable for post-acute stage. The causes for delayed initial evaluation were due to medical problems, such as respiratory tract infection, urinary tract infection, pressure sore, and deep vein thrombosis, inhibiting early rehabilitation therapy. Analyzed subjects consisted of 43 males and 19 females, and the average age was 49.6±18.4. Traumatic SCI patients (n=45) had their initial evaluation at 33.4±18.2 days after onset, and non-traumatic SCI patients (n=17) received initial evaluation at 41.3±20.6 after onset of injury. The number of subjects with tetraplegia was 36 and that of paraplegia was 26. Eighteen subjects had complete injury (ASIA A) while 44 subjects had incomplete injury (ASIA B, C, D).
ICF code linking process
ICF code linking process was carried out for the comprehensive evaluation records of 62 subjects. Principles for the linking process were established with reference to the ICF Red Book,11 "ICF application manual for users,"12 published by Statistics Korea, and several articles on the linking processes.9,10,13-15 Linking was done in the case of impairment of body function and structures, activity limitation, and participation restriction in the corresponding domains. For the environmental factors, linking was done in the case of both facilitators and barriers. Personal factors could not be linked to a specific code, thus, a separate description was done. For consistency, one experienced physiatrist performed the whole linking process.
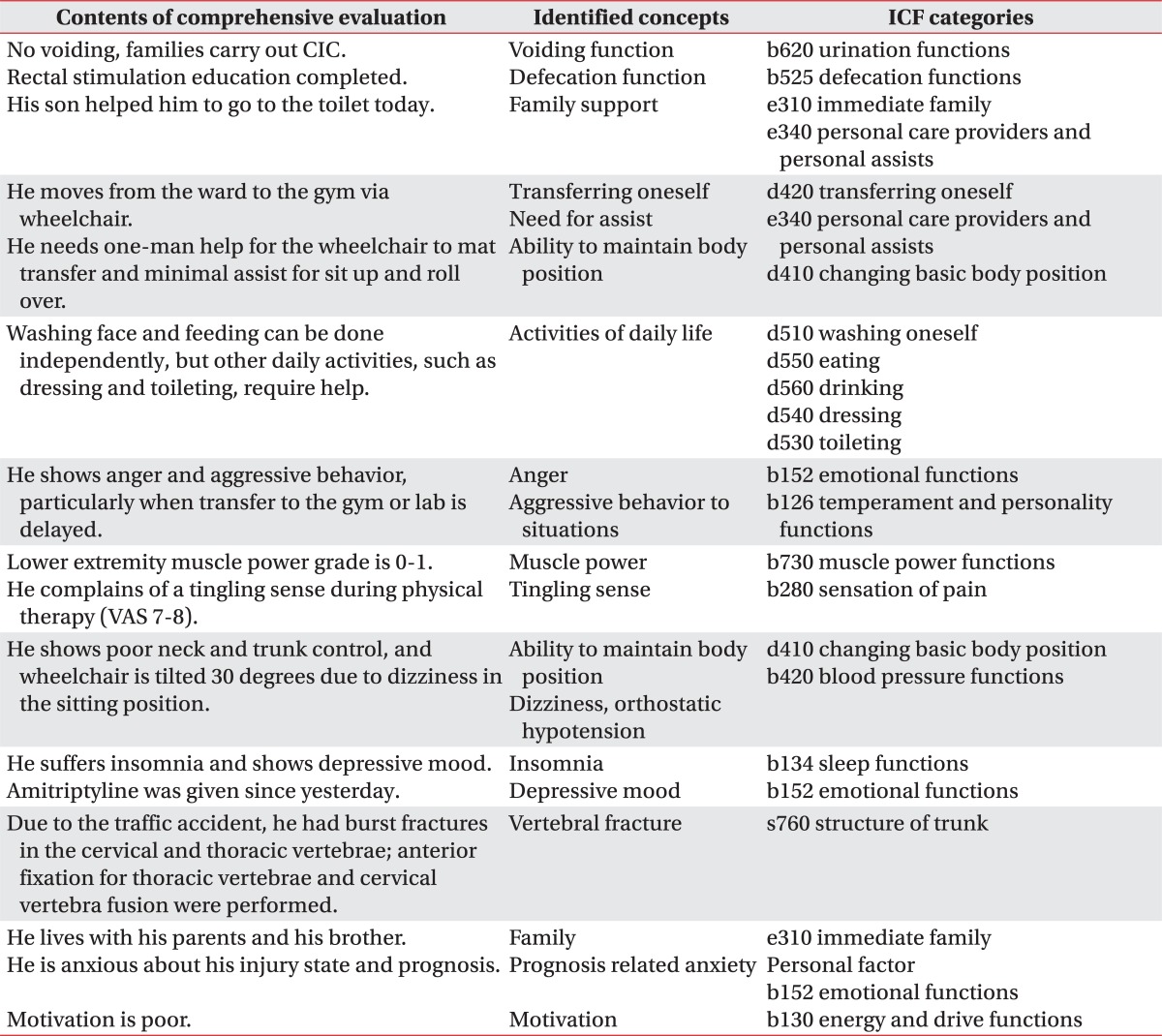
The linking process was performed in two steps.16 The first step was the identification of concepts, which was done by extracting the contents for linking from the records of the comprehensive evaluation. For example, in the description for the voiding and defecation function such as "family members perform clean intermittent catheterization (CIC) every 4-5 hours for the patient and the urine amount is about 200-500 cc every time," the concept of "family support" was deducted from the part that the family was helping the patient, and the "voiding function" was conceptualized for the fact that there was some problem in voiding. In the above example, simply, only the "voiding function" could have been conceptualized; however, in the comprehensive evaluation and rehabilitation, whether the family member, medical team, or the caregiver performs the CIC is an important factor, making it necessary to conceptualize "family support" in this case. The second step is the linking of concepts to the ICF. In the example described above, "family support (e310)" was linked for the help of family members, and the "urination function (b620)" was linked for the voiding problem. Other examples of the linking process are shown in Table 1.
Analysis
For the results of the linking process for the comprehensive evaluation, calculations for the linking frequency of each item for each domain were done. A comparison between the results of the ICF linking process and the ICF core sets was performed. Student's t test was used for the comparison between the type of injury and each domain. Descriptive analysis was used for personal factors.
RESULTS
Body functions
Nineteen items were linked in the body function domain. Muscle power functions (b730, 100%), urination functions (b620, 90.3%), sensation of pain (b280, 75.8%), and defecation functions (b525, 67.7%) were specifically linked frequently. Emotional functions (b152, 46.8%), protective functions of the skin (b810, 43.5%), weight maintenance functions (b530, 40.3%), energy and drive functions (b130, 38.7%), temperament and personality functions (b126, 30.6%), sleep functions (b134, 24.2%), ingestion functions (b510, 17.7%), blood pressure functions (b420, 14.5%), respiration functions (b440, 12.9%), and muscle tone functions (b735, 12.9%) were linked in the order of linked frequency. Items linked in less than 10% of the subjects were consciousness functions (b110, 6.5%), mental functions of language (b167, 4.8%), digestive functions (b515, 3.2%), intellectual functions (b117, 1.6%), and sensations associated with the digestive system (b535, 1.6%).
Body structures
In the body structures domain, 15 ICF 2nd level items were linked. The most frequently linked item was the spinal cord and related structures (s120, 100%), which was linked in all of the subjects. Yet, no other categories were linked in more than 10% of the subjects. The structure of respiratory system (s430, 9.7%), structure of brain (s110, 6.5%), and structure of urinary system (s610, 4.8%) were linked in the order of frequency. Other items were linked in less than 4 subjects.
Activities and participation
In the activities and participation domain, a total of 11 items were linked. Transferring oneself (d420, 96.8%), walking (d450, 93.5%), toileting (d530, 90.3%), dressing (d540, 88.7%), and washing oneself (d510, 87.1%) were frequently linked in more than 85% of the subjects. Changing basic body position (d410, 71.0%), hand and arm use (d445, 67.7%), drinking (d560, 58.1%), and eating (d550, 53.2%) were linked in more than 50% of the cases. Basic interpersonal interactions (d710, 16.1%) and remunerative employment (d850, 8.1%) were also mentioned several times.
Environmental factors
Nine items were linked in the domain of environmental factors. Immediate family (e310, 100%), health professionals (e355, 98.4%), and products and technology for personal indoor and outdoor mobility and transportation (e120, 95.2%) were highly linked frequently in more than 95% of the subjects. Individual attitudes of immediate family members (e410, 54.8%), assets (e165, 38.7%), personal care providers and personal assists (e340, 17.7%), social security services, systems and policies (e570, 17.7%), products and technology for personal use in daily living (e115, 12.9%), and friends (e320, 1.6%) were linked in the order of frequency.
Personal factors
For personal factors, specific ICF codes are not given for this domain. We described the contents for personal factors separately. The most frequently mentioned content was "insight on prognosis," which is important for all patients. This content was mentioned in 29.0% of the cases and was considered for setting the rehabilitation goals. In the cases that the patient did not know about the exact prognosis and expect much recovery of functioning despite the type of injury was complete, or in the cases that family members did not want to deliver the prognosis to the patient in concern that they will be shocked and lose motivation for rehabilitation, these were linked to personal factors as well as the corresponding body function and environmental factors. In these cases, difficulties in setting short-term and long-term rehabilitation goals were common. Suicidal ideas and attempts were also mentioned in several cases. Optimistic or pessimistic coping styles and behavioral patterns were also classified as personal factors.
Comparison with the ICF core set
The coverage rate of the brief ICF core set for contents of the comprehensive evaluation was 82.4±9.0%. The coverage rate for traumatic SCI and non-traumatic SCI were 82.5% and 81.9%, respectively, which did not show a statistically significant difference (p=0.806). The coverage rate for tetraplegia subjects and paraplegia subjects were 81.8% and 83.2%, respectively, which also did not show significant differences (p=0.539).
In the body function domain, the coverage rate of the brief ICF core set was 73.0%, and the other 27.0% of the contents consisted of items that were not included in the brief ICF core set. For the body structure domain, activities and participation domain, and environmental factors domain, the coverage rates were 87.3%, 96.0%, and 77.0%, respectively. There were no statistically significant differences between the coverage rates for each domain (p=0.302).
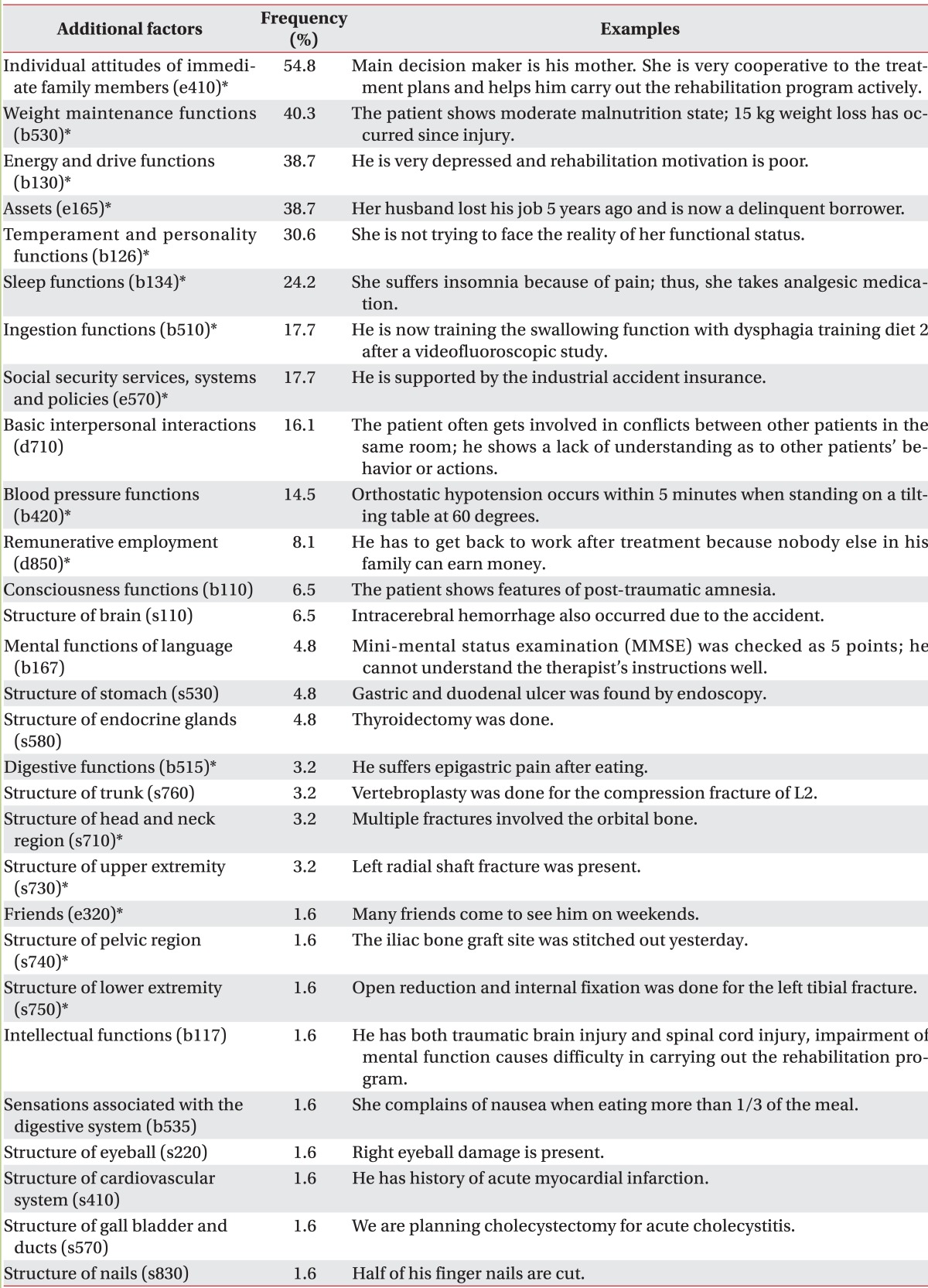
A total of 29 ICF 2nd level categories were linked in the comprehensive evaluation for rehabilitation but not included in the brief ICF core set. They consisted of 11 body function items, 12 body structure items, 2 activities and participation items, and 4 environmental factors. For the body function domain, weight maintenance functions (b530, 40.3%), energy and drive functions (b130, 38.7%), temperament and personality functions (b126, 30.6%), sleep functions (b134, 24.2%), ingestion functions (b510, 17.7%), and blood pressure functions (b420, 14.5%) were frequently linked items. There were no categories in the body structure domain that were linked frequently. Basic interpersonal interactions (d710, 16.1%) were frequently mentioned in the activities and participation domain. For the environmental factors domain, individual attitudes of immediate family members (e410, 54.8%), assets (e165, 38.7%), social security services, and systems and policies (e570, 17.7%) were often considered in the evaluation.
Of the 11 items that were additionally linked in the body function domain, 4 of them were not even included in the comprehensive ICF core set. In the body structure domain, 8 out of 12 additional linked factors were not included. One out of 2 items for the activities and participation domain were not included in the comprehensive ICF core set. For the environmental factors domain, all 4 of the additional factors were included in the comprehensive ICF core set.
Items that were linked to the ICF 2nd level categories, but not included in the brief ICF core set, are demonstrated in Table 2. Items that are included in the comprehensive ICF core set are marked with asterisks. Frequently linked categories were generally included in the comprehensive ICF core set ; however, basic interpersonal interactions (d710) were not included despite the linking frequency of 16.1%.
DISCUSSION
ICF is an international classification system to describe the health and health related status developed by the World Health Organization (WHO) in the year 2001 in order to enable a comprehensive and multidisciplinary approach to health and disability. ICF divides factors of health status as "functioning and disability" and "contextual factors." Functioning and disability is divided into the body functions and structures domain and the activities and participation domain. The contextual factors are divided into the environmental factors and personal factors. The ICF code is classified into 4 domains. First level classification consists of 30 items, second level has 362 items, and third to fourth level consists of 1,424 items.11
A brief ICF core set and comprehensive ICF core set has been published for post-acute SCI.2 The comprehensive ICF core set consists of 63 body function items, 14 body structure items, 53 activities and participation items, and 32 environmental factor items, with a total of 162 categories. Of these items, 8 body function items, 3 body structure items, 9 activities and participation items, and 5 environmental factors construct the brief ICF core set, with a total of 25 categories.
In this study, we hypothesized that a more systematic approach for acute SCI patients would be possible if the ICF classification is used in the initial comprehensive evaluation for rehabilitation. The aim of this study was to analyze the contents of the comprehensive evaluation records and compare it with the brief ICF core set, and to suggest a guideline for an initial approach for rehabilitation. There were many researches on the necessity of the ICF in a comprehensive evaluation; yet, to our knowledge, there were few researches on the practical usage of the ICF based on the analysis of clinical cases.
In our hospital, comprehensive evaluation is an important process that takes place within 1-2 weeks after patient admission to the rehabilitation unit. All rehabilitation team members that are involved in the rehabilitation process of the patient, such as physiatrists, physical therapists, occupational therapists, speech therapists, nurses, nutritionists, and medical social-workers, gather in one place to discuss the patient's status and establish short-term and long-term rehabilitation goals, and also make treatment plans. Prior to the year 2008, there were no specific forms for evaluation, and thus, each rehabilitation team member presented the patient's status in the view of their professionals, intuitively. For example, physiatrists mentioned medical problems primarily, physical therapists assessed on gait, muscle power, and joint problems, whereas medical social-workers focused on the socioeconomic aspects. From 2008, the evaluation form was established based on the ICF 1st level classification. With this form, every team members wrote their evaluation in each space according to the corresponding problem list and classification. More than one member could comment on the same problem list according to each member's point of view.
In the body function domain, muscle power functions, urination functions, defecation functions, and sensation of pain were frequently mentioned. These items involve problems that most of the SCI patients suffer, which is directly influenced by the spinal cord injury itself.17 Emotional functions, protective functions of the skin, weight maintenance functions, and energy and drive functions were categories that were mentioned in 40-50% of the subjects, which are secondary problems that occur because of impaired transfer and gait. Categories related to the primary effects mentioned above and the secondary effects, such as emotional functions and protective functions of the skin, are also included in the brief ICF core set, suggesting that these factors should always be evaluated.2 In contrast, weight maintenance functions and ingestion functions were not included in the brief ICF core set although many SCI patients complain of weight loss, dysphagia, and anorexia.18 Blood pressure functions were linked in 14.5% of the subjects, which is consistent with the fact that many SCI patients experience orthostatic hypotension during the attempt to stand after several days of bed rest. Orthostatic hypotension is a common symptom in post-acute SCI patients; hence, blood pressure should be considered in the process of rehabilitation and evaluation.19 Sleep function is also another important factor in the clinical environment, often presented as insomnia.18
In the body structure domain, spinal cord and related structures were linked in 100% of the subjects because all of the subjects included in this study were SCI patients. This suggests that the extent and location of the injury should be evaluated exactly by physical examination and by additional lab studies, such as MRI. The structure of the respiratory system and the structure of the urinary system had linking frequencies of 9.7% and 4.8%, respectively, mentioned in less than 10% of the subjects. In these cases, many subjects had impairment of related functions; however, these items were not linked if they did not go through tracheostomy or cystostomy. In Korea, patients or families tend to reject suggestions for tracheostomy and cystostomy, particularly within 90 days after injury onset. Respiratory and urinary structures are important, but personal and environmental factors seemed to make linking frequencies of these categories low.
In the activities and participation domain, items related with activities of daily lives were frequently mentioned. Transferring oneself, walking, toileting, washing oneself, and dressing had a high linking frequency of more than 85%, which are common problems in both tetraplegia and paraplegia. Categories related with mainly the upper extremity usage, such as hand and arm use, drinking, and eating, were linked in 50-60% of the subjects. Patterns of functioning and disability differ according to the level of injury, therefore, this must be considered in the evaluation.20 Most of the items in this domain were also included in the brief ICF core set except for basic interpersonal interactions and remunerative employment. This implies that most of the SCI patients suffer similar problems in the aspect of activities and participation.
In the environmental factor domain, "immediate family" who are primary caregivers, "health professionals" who are responsible for medical care, and "products and technology for personal indoor and outdoor mobility and transportation" which are important in overcoming the impaired transfer function, were very frequently linked, in over 95% of the subjects. In particular, the importance of family support and the social environmental factors were emphasized in many researches recently.21,22 These factors are also the important basis of the rehabilitation goal setting in our clinic.18
With regards to the personal factors, insight on prognosis was considered in 29.0% of the subjects, which was also an important factor in setting the rehabilitation goals. It would be ideal for the patient to know the current disease state and set realizable rehabilitation goals. However, in some cases, it was helpful for early rehabilitation by allowing the patient to realize the exact prognosis after some time has passed, considering the mental factors, age, occupation, and other environmental factors. Thus, in the comprehensive evaluation, all considerations should be taken into account in order to decide when to deliver the bad news to the patient. Kim and Shin23 reported that according to a survey based study, 44.1% of people answered that exact prognosis should be told to the patient within 1 months after injury, and 29.3% answered between 1 to 3 months.
For the personal factors in SCI, the individual's social status, personal history, emotion, thinking, belief, motivation, and behavioral patterns are the main factors that have to be considered.24 In this study, body function factors related with behavior, emotion, and mental status seemed to be overlapping with personal factors, making the linking process complicated. In this case, we linked those contents to the corresponding body function categories if proper category exists, and linked them to personal factors if not.
Overall, 82.4% of the evaluation contents were covered by the brief ICF core set. In other words, 17.6% of the evaluation could have been omitted if the evaluation was only performed by the brief core set. Particularly in the activities and participation domain, the coverage rate of the brief ICF core set was high as 96%, which seemed to be due to the fact that most of the SCI patients suffer similar situations regarding activities of daily lives, and these items became the main focus in the comprehensive evaluation. The coverage rates of the brief ICF core set in the body function domain (73.0%) and environmental factor domain (77.0%) are lower than the average. Different underlying diseases or medical conditions as well as various economic and social backgrounds of each patient could be a good explanation for this disparity. Many contents, other than the brief ICF core set items, have been mentioned during the comprehensive evaluation process in the body function and environmental factor domains.25 The linking frequency of the brief ICF core set categories are listed in Table 3. The additional factors that were discussed in the comprehensive evaluation, but not included in the brief ICF core set, are listed in Table 2, in the order of linking frequency.
The time standard for the period of acute spinal cord injury is not exactly defined. However, Sumida et al.26 suggested that the neurologically acute stage is until 1 week after the onset of injury, subacute stage is from 2 weeks to 4 weeks after injury, and that 3-6 months after injury is the chronic stage when the neurological recovery rate is slowed down. Wuermser et al.17 stated that most of the neurological recovery process takes place within 3 months after injury. Integrating the above opinions, we can consider that initiating rehabilitation at least within 3 months after the injury onset is appropriate in order to designate the rehabilitation as "post-acute rehabilitation." In this study, the average post-onset duration for the initial comprehensive evaluation was 33.4±18.2 days for traumatic SCI patients and 41.3±20.6 days for non-traumatic patients, which was suitable for regarding the rehabilitation of the patients as "post-acute rehabilitation."
There were several advantages in using the problem list oriented comprehensive evaluation based on the ICF 1st level classification from year 2008, compared to the evaluation based on the point of view of each rehabilitation team members. First, sharing detailed information for each problem was possible. For example, for the "transfer" function, the physical therapist described the mat activity pattern, the nurse described the situation of bed to wheelchair transfer, while the doctor gave information on muscle power and spasticity, making it possible for all members to have a three-dimensional concept on the transfer function. Second, more definite and realistic rehabilitation goal could be set according to the problem list. For instance, in the voiding function, it could be difficult to decide whether clear intermittent catheterization or indwelling foley catheter is more appropriate. In these cases, not only the patients themselves, but doctors, medical social-workers, nurses, and occupational therapists shared their opinions based on their point of view, and made the most appropriate decision for the current situation.27
There were also some limitations to this study. The linking process was done only according to whether the contents corresponding to the 2nd level ICF category were mentioned or not, and the ICF qualifiers were not used for the analysis. Thus, the degree of significance for the linked ICF categories in individual patients was not reflected in the analysis. Unfortunately, we could not make task assignments for rehabilitation team members using the ICF based on our results, or make outcome measurements after the rehabilitation treatment. These topics should be considered in future studies.
In this study, we aimed to investigate the utility of the ICF classification and the ICF core set for problem list oriented comprehensive evaluation. But according to the analysis, 17.6% of the comprehensive evaluation contents were not covered by the brief ICF core set. Hence, we need to make an evaluation system as not to omit the additional contents because the brief ICF core set cannot fully substitute the comprehensive evaluation alone. Therefore, for the initial comprehensive evaluation for rehabilitation of SCI patients, we should maintain the problem list oriented framework based on the ICF 1st level classification, and provide the factors of the ICF 2nd level categories that were linked with the high frequency in the evaluation as a checklist. There were several contents that were essential for patient evaluation but not included in the brief ICF core set. Moreover, 44% of the additional factors were not even included in the comprehensive ICF core set; therefore, an evaluation framework with an open question form based on the ICF 1st level classification is necessary.
There have been researches for the utility of ICF in other disease categories. For head and neck cancer, Tschiesner et al.28 stated that an evaluation tool covering all the situations and symptoms could not exist, yet, the ICF could be a definite tool to help standardize and structurize the evaluation of functioning. In a prospective cohort study for post-acute rehabilitation of 116 musculoskeletal, neurological, and cardio-respiratory patients, Lohmann et al.27 insisted that 426 items (78%) out of 546 linked items in the comprehensive evaluation corresponded to the ICF core set; hence, ICF could be helpful for setting rehabilitation goals, yet, the patient's perspective should be considered additionally.
CONCLUSION
ICF can provide a structural framework for the problem list oriented comprehensive evaluation in rehabilitation. Categories of the brief ICF core set, additional factors mentioned in this study, as well as the personal factors should be considered for the evaluation. Therefore, we should maintain the current framework based on the ICF 1st level categories so that omission of essential contents could be prevented. Additionally, items of the brief ICF core set, additional factors that were frequently mentioned in this study, and personal factors should be provided as a checklist. This would be helpful for the systematic and comprehensive evaluation and serve as a basis for adequate and realistic rehabilitation goal setting.