A Pulmonary Telerehabilitation Program Improves Exercise Capacity and Quality of Life in Young Females Post-COVID-19 Patients
Article information
Abstract
Objective
To examine the impact of telerehabilitation training on exercise capacity, lung function, and health-related quality of life (HRQOL) in comparison to no rehabilitation for post-COVID-19 symptoms in adult females.
Methods
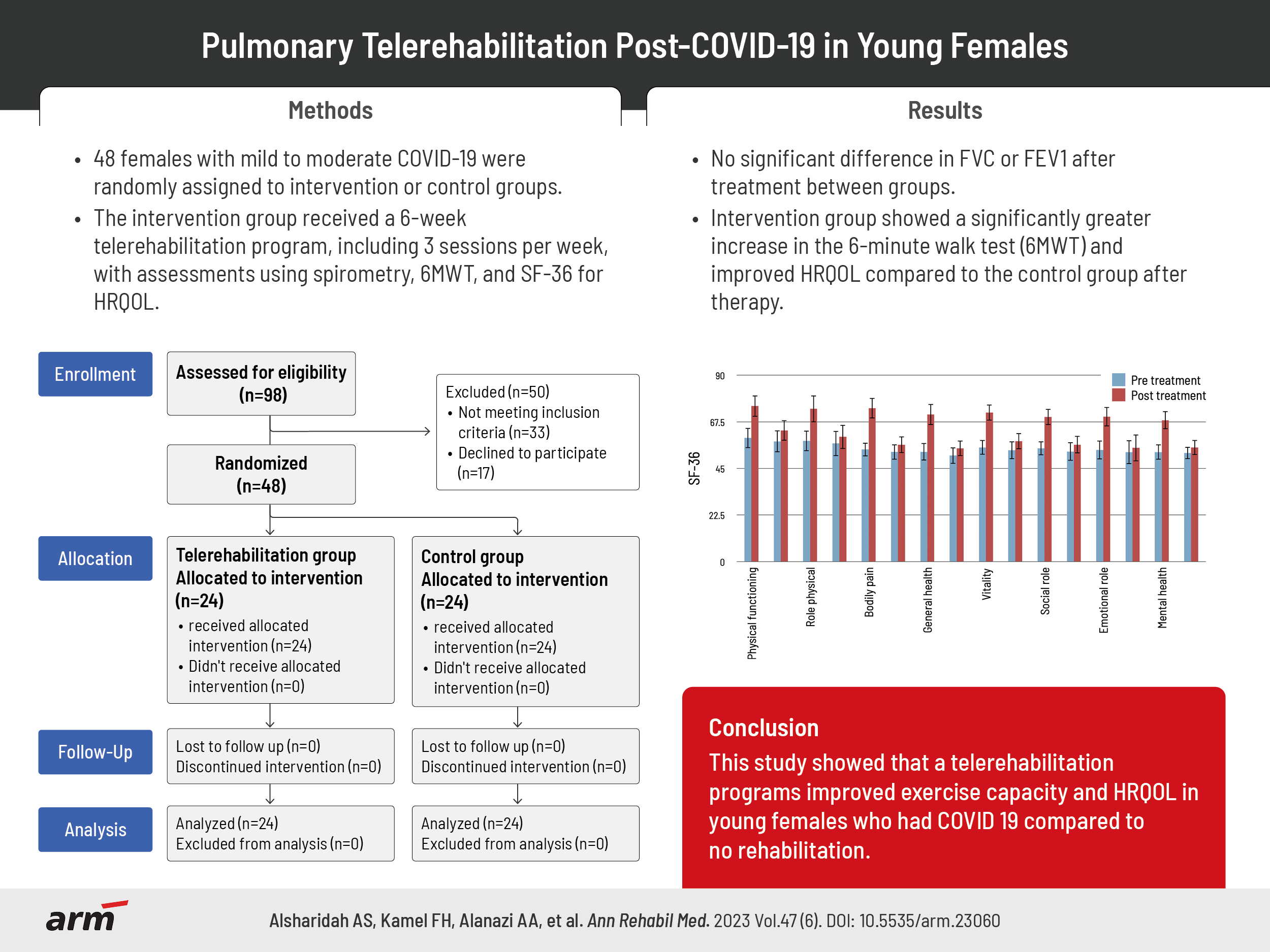
A randomized controlled trial of 48 females after mild to moderate COVID-19 survival were equally and randomly assigned to one of two groups: intervention group or control group. Three sessions per week for 6 weeks of a telerehabilitation program provided via a smartphone to the intervention group. Spirometry was used to quantify lung function, a 6-minute walk test (6MWT) measured in meters to measure exercise capacity, and the Short Form Health Survey-36 was used to assess HRQOL.
Results
After treatment, there was no statistically significant difference in forced vital capacity (FVC) or forced expiratory volume in 1 second (FEV1) between groups (p>0.05), but the 6MWT of the intervention group increased significantly more than that of the control group (p=0.001). The percent of change in 6MWT for the intervention group and control group was 14.22% and 4.21%, respectively. After therapy, the intervention group’s HRQOL significantly improved when compared to the control group’s (p=0.001).
Conclusion
This study showed that a telerehabilitation programs improved exercise capacity and HRQOL in young females post-COVID-19 compared to no rehabilitation.
INTRODUCTION
In addition to the acute morbidity and mortality of coronavirus disease 2019 (COVID-19) infection, survivors of COVID-19 have also experienced post-acute health complications and repercussions. A review found that more than 50 adverse effects were observed, and that up to 80% of COVID-19 patients continue to experience health issues following an acute infection. Several post-acute symptoms still have unclear pathophysiologies. Thought to be a major mediator in the multifactorial development of the long-term consequences, ongoing inflammation is still seen as a problem [1].
The term “post-acute sequelae” COVID-19 refers to a broad variety of health issues that follow an acute infection [1-3]. Individuals who have COVID-19 post-acute sequelae experience new, reoccurring, and persistent symptoms four weeks or longer well after the infection [2]. Several guidelines describe the time point for the post-acute stage as ranging between approximately four weeks and three months following the infection [4,5]. The term “long COVID syndrome” generally refers to signs and symptoms that persist or worsen after an initial COVID-19 infection and may take months to resolve completely [6,7]. There are variations in the reported prevalence of long-COVID syndrome across studies and nations [3,8,9]. These manifestations usually include, but are not restricted to, dyspnea, pain, exhaustion, breathing difficulty, compromised lung function, muscle weakness, restricted exercise tolerance, confusion and depressed mood, impaired memory, poor concentration (“brain fog”), neurological problems, taste/smell abnormalities, and poor health-related quality of life (HRQOL) [1-3].
To improve awareness and, particularly, access for those in distant communities or who face transportation challenges, the adoption of telemedicine services has lately been explored as an additional and novel method of providing rehabilitation to patients in their households. An at-home rehabilitation using telemonitoring technology offers considerable potential for preserving and enhancing functional capacity [10].
The burden of long-term COVID is rising rapidly, necessitating the development of interventions to enhance patient long-term outcomes. Presently, policy documents and recommendation statements support both short- and long-term rehabilitation [11,12]. These suggestions, however, are dependent solely on consensus opinion and lack data from specific trials examining the positive impacts of inpatient or outpatient rehabilitation in individuals experiencing long-term health complications following COVID-19.
Others made a significant observation that women and those who had more severe acute infections were more likely than men to experience most manifestations and symptom clusters, and that post-COVID syndrome also impacted younger individuals. Females aged ≥20 years were more likely to have long-COVID symptoms than males aged ≥20 years (10.6% vs. 5.4%) [13,14]. Therefore, the purpose of this study was to evaluate the outcomes of a home-based pulmonary training program (including aerobic, resistance, and breathing exercises) under the supervision of telerehabilitation on pulmonary function, exercise tolerance and HRQOL in participants who had COVID-19 manifestations.
METHODS
Study design
The research was carried out between December 2021 and June 2022. All study participants submitted informed consent in writing to participate in this trial. Qassim Regional Research Ethics Committee (No. 784946-1443) approved all study protocols which were carried out in line with the Declaration of Helsinki. The investigation was prospectively listed on ClinicalTrials.gov (NCT05172102).
Participants
After a positive nasopharyngeal or oropharyngeal swab verified the diagnosis of COVID-19, participants were sought out from females at Qassim University in Kingdom of Saudi Arabia via brochures, social media, and online platforms. When the participants expressed willingness to participate, a researcher confirmed their possible candidacy and set up a face-to-face meeting to complete the baseline evaluation. The following in-person appointments were arranged for follow-up evaluations at the baseline assessment. All the testing procedures were performed at cardiopulmonary lab in college of medical rehabilitation, Qassim University. The study included mild to moderate post-COVID-19 survivors, COVID-19 severity was classified into three categories mild to moderate (outpatients with a flu-like condition or probable pneumonia), severe (hospitalized patients treated in hospital wards), and critical (patients treated in an intensive care unit) [15], 18 to 30 years old, not smokers, with a body mass index (BMI) between 18.5 and 24.9 kg/m2.
Candidates were excluded if they had any of the following: (1) an identification of progressive neuromuscular, respiratory, or neurological conditions; (2) a contraindication to pulmonary rehabilitation intervention such as angina pectoris, recent myocardial infarction, severe pulmonary hypertension, congestive heart failure, unstable diabetes, inability to do exercise due to orthopedic as intra-articular drug injection or surgical treatment of lower extremities, psychiatric illness and severe exercise-induced hypoxemia [16]; (3) no internet service; or (4) previous participation in a rehab program following a COVID-19 condition. A further exclusion applied to participants who missed more than 15% of therapy sessions.
Sample size calculation was performed using G*Power statistical software (version 3.1.9.2) based on data of 6-minute walk test (6MWT) derived from pilot study conducted on 5 subjects in each group; and revealed that the required sample size for this study was 20 subjects in each group. Calculation is made with α=0.05, power=80% and effect size=0.91, For dropout the sample increase to 20%. Participants were randomized and divided into two groups using a simple random approach, and the findings were packed into opaque envelopes to keep the order of group assignment from the investigator who recruited the participants undisclosed. The control group (n=24) received standardized educational instructions and the intervention group received telerehabilitation pulmonary exercise program (n=24) for 6 weeks. It was not possible to blind the treating therapists who participated in the study due to the nature of study procedures. The evaluating therapist was blinded when evaluating the outcomes initially and after the intervention. The treatment and evaluation therapists were different, and the evaluating therapists kept blind of the participants. The participants were instructed not to share their procedures and treatment plan with the therapist who would be evaluating them.
Control group
The participants in the control group got written instructions on an explanatory note and prescribed educational presentations from physiotherapists for 10 minutes. They were instructed to continue with their regular everyday routines, refrain from prolonged bed rest and immobility, engage in light physical activity, such as housework, follow a balanced diet, and get 6 to 8 hours of sleep each night. Also, patients were given instructions on proper facemask use, social distancing, and essential hand hygiene.
Intervention group
In addition to receiving the same instructions and informational materials as the control group, the intervention group also participated in a home exercise routine that was virtually supervised and given via telerehabilitation. The duration of the intervention program was 60 to 80 minutes per session, three sessions per week for 6 weeks.
To ensure safety, proper and correct exercise technique, small groups of 2 to 6 participants underwent the session at a time for education, supervised by specialized physical therapist at college of medical rehabilitation, Qassim University. Telerehabilitation program was guided by a specialized physical therapy professional through a web platform (by Zoom Video Communications), in live sessions. Participants were asked to connect themselves to the platform in groups of 5 participants, three times a week, for 6 weeks. Each week, the therapist indicated and corroborated individually to each patient the load with which she should train.
Initial exercise types and intensity were determined by the physical therapist based on baseline assessments and in accordance with the American College of Sports Medicine’s recommendations for exercise prior to participation [17]. The telerehabilitation pulmonary exercise regime contained (1) breathing exercises and chest expansion, including diaphragmatic breathing exercise, as well as other activities aimed to enhance chest wall muscle strength and chest mobility for 15 minutes. (2) Aerobic activity for 20 to 30 minutes consisted of brisk walking or running outside close to the participant’s home or using a treadmill at home (if one was accessible), accompanied by a 3-minute warm-up and 3-minute stretching cool-down. At exercise intensity between 60% and 80% of maximal heart rate, which was defined as 220 minus age [18], the target heart rate for aerobic exercise was determined using the Karvonen formula [19], patients were asked to self-monitor during aerobic exercise and were also trained for reporting Borg scale themselves, and (3) resistance training with weights was proposed to the participants based on an individual’s personal evaluation for 30 minutes.
Ten-repetition maximum was used to determine the ideal resistance needed for each muscle group, and the DeLorme method was used to train the muscles [20]. The most weight that a subject can lift repeatedly for ten repetitions is known as the 10-repetition maximum. The main group muscles, including the back, abdominal, shoulder (flexors, extensors, abductors), elbow, hip and knee (flexors, extensors) were exercised. Every muscle group received three sets of 10 repetitions each, with a 60-second rest between sets. In accordance with each person’s needs, the resistance was gradually increased.
To maintain clinical safety limits, respiratory rate, heart rate, oxygen saturation (SpO2), and Borg scale were monitored at each session. Patients were asked to acquire a pulse oximeter to measure their SpO2 and to self-monitor during the sessions and were also trained for reporting Borg scale themselves. If the SpO2 value decreased by 4% and if it fell below 95% or registered an increase of three points with respect to the initial value of the Borg scale, the participant had to interrupt the session. Other reasons for interrupting the session were an increase in heart rate by 20 beats per minute, dizziness, sweating, headache, or chest pressure.
To record compliance, participants were asked to complete a diary at the end of every training session. Adherence to the program was assessed and confirmed by comparing the physiotherapist’s notes against each participant’s diary notes.
Measurements
Assessment of outcomes for each group was conducted at baseline (pretreatment) and after 6 weeks of intervention (posttreatment). Assessment of functional exercise capacity was conducted using the 6-MWT. According to recommendations from the American Thoracic Society and the European Respiratory Society (ATS/ERS), the 6-MWT was carried out in a 30-meter corridor with standard guidelines. After the 6-MWT, the walking distance was measured [21].
In accordance with the recommendations of ATS/ERS [22], pulmonary function evaluated using spirometry (SpirOx; MEDITECH). The forced expiratory volume in 1 second (FEV1) and the forced vital capacity (FVC) are the two spirometric tests that will be performed. There will be three successful attempts. The best trial out of the three will be considered.
HRQOL was assessed using the Short Form Health Survey-36 (SF-36) questionnaire, which has been validated. Physical functioning, bodily pain, social functioning, general health, role-physical, role-emotional, vitality, and mental health are the eight scales that make up the SF-36, which consists of 36 items in total. Item scores are recorded, added up, and converted to a scale from 0 (lowest health status) to 100 (best health status) based on these parameters. We used the tool’s Arabic version, which has been found to be reliable and accurate [23].
Statistical analysis
The comparison of subject characteristics between groups was done using an unpaired t-test. Shapiro–Wilk test was used to determine whether the data is normally distributed. The homogeneity between groups was examined using Levene’s test for homogeneity of variances. Mixed MANOVA was used to examine how the intervention affected the 6MWT, FVC, FEV1, and SF-36. For further multiple comparisons, post-hoc testing employing the Bonferroni correction were conducted. All statistical tests had a significance threshold of p<0.05. The IBM SPSS version 25 for Windows (IBM Corp.) was used for all statistical analysis.
RESULTS
The flow of subjects through the research is depicted in Fig. 1. In this study, 48 participants took part in this trial and 50 participants were excluded from the study (33 participants do not meet the inclusion criteria of the study and 17 participants declined to participate). The treatment adherence rate for intervention group was 94.21%, with participants completing 16.96±0.86 sessions. The subject characteristics for the intervention group and control group are displayed in Table 1. Age, BMI, and period of rehabilitation following confirmed COVID-19 did not significantly differ between groups (p>0.05).
A significant interaction effect of intervention and time was identified by mixed MANOVA (F=413.09, p=0.001). There was a significant main effect time (F=942.28, p=0.001). There was a significant main effect of intervention (F=32.78, p=0.001).
Before treatment, there was no detectable difference between the groups (p>0.05). Posttreatment comparisons between the groups showed no significant differences in FVC or FEV1 between the groups (p>0.05), while the intervention group significantly increased its 6MWT compared to the control group (p=0.001; Table 2).
Following treatment, there was a statistically significant difference between the intervention group and the control group in terms of physical functioning, bodily pain, social functioning, general health, role-physical, role-emotional, vitality, and mental health (p=0.001; Table 3, Fig. 2).

Mean Short Form Health Survey-36 (SF-36) pre- and posttreatment of group A (intervention group) and B (control group).
In the intervention group, there was a 25.88%, 26.57%, 36.97%, 34.04%, 30.58%, 27.62%, 29.82%, and 29.24% changes in physical functioning, role physical, bodily pain, general health, vitality, social role, emotional role and mental health respectively.
DISCUSSION
In this trial, exercise capacity, pulmonary function, and HRQOL in females with post-COVID-19 symptoms were examined in relation to a home-based pulmonary training program that was videoconference-monitored. The findings of this study demonstrated that the pulmonary training program was successful in enhancing HRQOL and exercise capacity. There were no changes in the parameters of lung function after the pulmonary training program. The intervention protocol was adhered effectively, and there were no significant adverse events.
In this study, a patient-centered, customizable inexpensive telerehabilitation intervention was assessed using a variety of measures that were pertinent to exercise capacity, lung function, and HRQOL. The availability of therapists for remote supervision and consultations, smartphone access, technological literacy, are all factors supporting the suitability of telerehabilitation programs for large-scale deployment. When a face-to-face program cannot be conducted, telerehabilitation has been suggested as a reasonable alternative. An at-home telerehabilitation program for patients with post-COVID-19 fatigue, which included aerobic and strength training, had positive effects on their persistent symptoms as well as on physical capacity or walking distance measurements [24].
The patients in this study had mild to moderate COVID-19, but they also had significant restrictions. Recovery is frequently incomplete and sluggish. In young adults and people with no or few chronic underlying medical illnesses, mild to moderate nonhospitalized COVID-19 disease can cause extended sickness and persistent symptoms [25,26].
The physical capacity of post-COVID-19 patients is moderately impaired, which is likely due to muscle deconditioning, according to earlier studies [27,28]. Other contributing factors to the overall symptomatology include physical deconditioning and decreased exercise tolerance [29-31]. Furthermore, immobility forced by hospital stays and/or enforced quarantine at home worsens the clinical presentation and symptoms in these patients, who may experience symptoms that persist for a long time after having COVID-19 disease [32]. Moreover, the 6MWT was at 76% of the expected capacity among patients who reported physical and psychological consequences in a 5-year follow-up study on 109 acute respiratory distress syndrome survivors [33].
Participants in this trial increased their 6MWT by almost double the minimal clinically important difference, which is about equivalent to rehabilitation outcomes in other COVID-19 patients [34,35]. It appears that referring COVID-19 patients to pulmonary rehabilitation following the acute phase of the disease can facilitate the recovery of exercise capacity. Exercise capacity both in the physical and mental components of HRQL exhibited similar improvement. Like in other studies [34,35], the influence on quality of life was statistically significant when comparing to the control group.
Patients displayed a lower FEV1 at baseline, which is consistent with another research on post-COVID-19 [36]. Breathing exercises have been shown to have superior effects on lung function measures (FEV1 and FVC) compared to controls for chronic obstructive pulmonary disease (COPD) in a recent systematic review and meta-analysis [37], but no such effects were observed in the current investigation. In the intervention group, both parameters (i.e., FVC and FEV1) significantly improved throughout the course of the 6-week rehabilitation period; nevertheless, no significant between-group variation was observed. Additionally, it was determined that the intervention group’s mean differences FEV1 was 0.17 and percentage of change was 7.66% of baseline, and the mean difference of FVC was 0.21 and percentage of change was 7.75% of baseline, did not exceed the clinically meaningful change threshold for patients with COPD that is advised by ATS/ERS (week to week). One possibility is that the workouts used in the intervention program did not substantially target lung function. Further Li et al. [34] findings add evidence to this perspective.
Cardiopulmonary-rehabilitation programs recently emerged to be advised in the treatment of patients following COVID-19 to address the significant disability of people with prolonged COVID-19 and the decline in their quality of life [12,38,39]. Guidelines in this direction were released in 2020 by the Pan American Health Organization, a member of the World Health Organization, for both patients who had COVID-19 in its acute phase and those who were still experiencing its long-term effects [40]. Customized rehabilitation-training regimens include cardiopulmonary activities, muscle-strengthening exercises, and focused breathing techniques may improve recovery.
While interpreting the results of our study, it is important to consider many limitations. First, only mild to moderate COVID-19 survivors who had never been hospitalized were included in participant characteristics. The lack of data for some of the secondary outcomes, such as dyspnea, level of fatigue, inspiratory muscle strength, etc., limits the scope of our study. Second, the research cohort was young, highly educated, and most likely had a strong network of healthcare providers, their referrals to rehabilitation without defined protocols at the time cannot be extended to the entire population of COVID-19 survivors. Finally, the small patient population made it difficult to do subgroup analyses to look at variations in illness outcome and progression according to patient variables.
In conclusion, the telerehabilitation pulmonary program is superior to no rehabilitation with regarding to exercise capacity and HRQOL in young females after long COVID-19. The effect of the programs on pulmonary function is otherwise unlikely. In sum, our research affirms the efficacy of integrated customized rehabilitation for COVID-19 young female only. Future studies should focus on the long-term consequences of rehabilitation and the apparent improvement in pulmonary function in other age and sex.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING INFORMATION
None.
DATA AVAILABILITY STATEMENT
The authors declare that all relevant data supporting the findings of the study are available within the manuscript.
AUTHOR CONTRIBUTION
Conceptualization: Basha MA, Alrshedi ZO. Data curation: Alanazi AA, Alhawsah EA, Alharbi HK. Formal analysis: Kamel FH, Basha MA. Investigation: Alanazi AA, Alhawsah EA, Alharbi HK, Alrshedi ZO. Methodology: Alsharidah AS, Kamel FH, Basha MA. Project administration: Basha MA. Resources: Alanazi AA, Alhawsah EA, Alharbi HK, Alrshedi ZO. Software: Basha MA. Supervision: Basha MA. Validation: Alsharidah AS, Kamel FH. Visualization: Alsharidah AS, Kamel FH. Writing – original draft: Alanazi AA, Alhawsah EA, Alharbi HK, Alrshedi ZO, Basha MA. Writing – review editing: Alsharidah AS, Kamel FH, Basha MA. Approval of final manuscript: all authors.
Acknowledgements
The authors appreciate all the participants for making this study possible.