Clinical Practice Guidelines for Oropharyngeal Dysphagia
Article information
Abstract
Objective
Dysphagia is a common clinical condition characterized by difficulty in swallowing. It is sub-classified into oropharyngeal dysphagia, which refers to problems in the mouth and pharynx, and esophageal dysphagia, which refers to problems in the esophageal body and esophagogastric junction. Dysphagia can have a significant negative impact one’s physical health and quality of life as its severity increases. Therefore, proper assessment and management of dysphagia are critical for improving swallowing function and preventing complications. Thus a guideline was developed to provide evidence-based recommendations for assessment and management in patients with dysphagia.
Methods
Nineteen key questions on dysphagia were developed. These questions dealt with various aspects of problems related to dysphagia, including assessment, management, and complications. A literature search for relevant articles was conducted using Pubmed, Embase, the Cochrane Library, and one domestic database of KoreaMed, until April 2021. The level of evidence and recommendation grade were established according to the Grading of Recommendation Assessment, Development and Evaluation methodology.
Results
Early screening and assessment of videofluoroscopic swallowing were recommended for assessing the presence of dysphagia. Therapeutic methods, such as tongue and pharyngeal muscle strengthening exercises and neuromuscular electrical stimulation with swallowing therapy, were effective in improving swallowing function and quality of life in patients with dysphagia. Nutritional intervention and an oral care program were also recommended.
Conclusion
This guideline presents recommendations for the assessment and management of patients with oropharyngeal dysphagia, including rehabilitative strategies.
INTRODUCTION
Dysphagia is a common clinical condition characterized by difficulty in swallowing. It is sub-classified into oropharyngeal dysphagia, which refers to problems in the mouth and pharynx, and esophageal dysphagia, which refers to problems in the esophageal body and esophagogastric junction [1]. Oropharyngeal dysphagia is characterized by difficulty in initiating a swallow or passing food through the mouth or throat [2], whereas esophageal dysphagia accompanies structural or inflammatory abnormalities or motility disorders [3].
Dysphagia is associated with an acquired health condition, such as stroke, Parkinson’s disease, or motor neuron disease, as well as developmental disabilities. The prevalence of dysphagia is estimated to be 8% of the world’s population, and its prevalence increases in the older adult population [4]. The prevalence of dysphagia in older people dwelling in communities is approximately 15% and approximately 30% in hospitalized patients [1]. It occurs most commonly in old patients with neurological disorders and dementia, with a prevalence of 64% and 80%, respectively [5].
Dysphagia can have a significant negative impact on one’s physical health and quality of life as its severity increases [6]. If dysphagia is not properly evaluated and timely treated, it may worsen the quality of life and cause serious complications, such as dehydration, malnutrition, and aspiration pneumonia. Importantly, oropharyngeal dysphagia should be identified promptly considering the risk of aspiration. Various interventions such modifying food textures, positioning modification, or rehabilitative and compensatory strategies are designed to improve swallowing efficiency and reduce the risk of complications in patients with dysphagia [7].
Purpose of clinical practice guidelines
The purpose of this clinical practice guideline (CPG) was to provide a guideline supported by scientific evidence for physicians and other healthcare professions who diagnose and treat patients with symptoms of dysphagia. This CPG is aimed to assist in decision-making for appropriate treatment options to improve the clinical outcome of patients with dysphagia and reduce extravagant costs to patients and the overall health care system.
Scope of CPGs
Assessment and management of dysphagia are mainly addressed in this CPG. Patients with progressive neurological disease and under 18 years of age were excluded from the scope of this CPG. This guideline does not aim to limit physicians’ medical practices and is not used to evaluate the quality of their practices.
METHODS
CPG development group
The development group involved a development committee and an advisory committee, including three methodology experts. The development committee members consisted of 45 physicians (25 physiatrists, 15 otorhinolaryngologists, 2 gastroenterologists, and 3 dentists), 2 nursing staff, 3 nutritionists, 3 occupational therapists, and 2 language therapists. For each key question (KQ), 55 development committee members determined the level of evidence and recommendation level.
KQs
This CPG consists of four categories: (1) assessment, (2) treatment, (3) nutritional management, and (4) complications and others. KQ was determined based on the Population Intervention Comparator Outcome (PICO) framework. According to the PICO strategy, adult patients of the population group who have symptoms or diagnosis of oropharyngeal dysphagia were included in this guideline. The number of KQs was determined by the number of interventions. The majority of outcomes focused mainly on improvement of dysphagia. If necessary, KQs were further divided into sub-KQs. Finally, a total of 19 KQs were formulated for this guideline.
Search strategy
A literature search was conducted for relevant articles using PubMed, Embase, the Cochrane Library, and one domestic database of KoreaMed, until April 2021. After establishing a highly sensitive strategy in combination with the natural language, the MeSH term was also used for PubMed and Cochrane Library, and the Emtree term was used for Embase (Supplementary Data 1).
The search results were collated in EndNote. For each KQ, two independent reviewers excluded articles that did not meet the inclusion criteria of this CPG after reading titles and abstracts. Furthermore, full-text assessments were followed to reject those that did not fulfill the inclusion criteria. Articles that included patients with progressive neurological diseases (e.g., Parkinson’s disease or dementia) and patients who were under 18 years of age were excluded. We also included articles written in languages other than English or Korean, articles that exist only in abstract form, case reports, technical reports, and animal studies. Study screening and data extraction were independently performed by two reviewers. The reviewers attempted to resolve any disagreement by consensus. If necessary, the opinion of a third reviewer was put into consideration to resolve the disagreement.
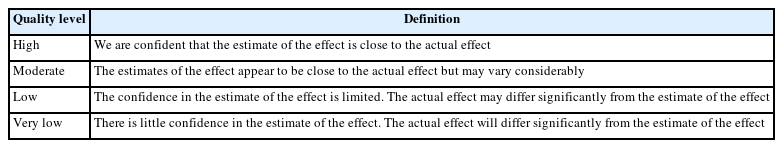
Quality assessment was performed on selected articles. The bias assessment was conducted using Cochrane risk-of-bias 2.0 for randomized controlled trials (RCTs) and the risk-of-bias assessment tool for non-randomized studies for non-RCTs [8,9]. The methodological quality of the systematic reviews (SRs) was evaluated using AMSTAR 1.0—a measurement tool to assess the methodological quality of SRs [10] (Supplementary Data 2). The level of evidence and recommendation grade were established according to the Grading of Recommendation Assessment, Development and Evaluation (GRADE) methodology [11]. The level of evidence was evaluated by assessing the degree of bias, consistency, directness, accuracy, and publication bias in the RCTs, non-RCTs, and SRs. The level of evidence for each KQ was based on the GRADE methodology as “high,” “medium,” “low,” and “very low” (Table 1). The level of recommendation was determined according to a modified GRADE methodology divided into four levels (Table 2). Several factors were considered, including the level of evidence, balance of benefits and harms, values and preferences, obstacles and facilitating factors, resource and cost, and clinical applicability. The KQs that could not be further developed due to poor existing research were represented as expert consensus.
Grading of Recommendations Assessment, Development and Evaluation quality level of evidence and meaning
For each KQ, at least two members of the development group participated in formulating and reviewing the draft recommendations. The working members continued discussions to reach consensus, and revisions were made there after in accordance with the opinions of the advisory committee. The recommendations were also revised through a review process via e-mail and a wired meeting with experts in the relevant field, and a formal consensus was achieved. The level of evidence and recommendations for 19 KQs were evaluated, and the content of the recommendations and the recommendation grade was adjusted through in-depth discussion. The degree of consent for each committee member was selected from one (non-acceptance) to nine (acceptance) on a nine-point scale. If the score was ≥7, consent was considered to be present. If at least 75% of the committee members agreed to the final version of the recommendations, it was deemed to have reached a consensus. Finally, the final version of the 19 recommendations was accepted. This guideline will be revised every 5 years, when there is solid evidence that it can affect the management and treatment of patients with oropharyngeal dysphagia.
RESULTS
Summary of recommendations
1. Assessment of oropharyngeal dysphagia
KQ 1. Early screening
A. Evidence level: high
B. Grade of recommendation: strong
KQ 2. Standardized screening test
A. Evidence level: not applicable
B. Grade of recommendation: expert consensus
KQ 3. Videofluoroscopic swallowing study (VFSS) vs. clinical evaluation
A. Evidence level: moderate
B. Grade of recommendation: strong
KQ 4. VFSS vs. fiberoptic endoscopic examination of swallowing (FEES)
A. Evidence level: inconclusive
B. Grade of recommendation: inconclusive
2. Treatment for oropharyngeal dysphagia
KQ 5. Oropharyngeal sensory stimulation
A. Evidence level: low
B. Grade of recommendation: conditional
KQ 6. Exercises
KQ 6.1. Tongue and pharyngeal muscle strengthening exercise
A. Evidence level: moderate
B. Grade of recommendation: strong
KQ 6.2. Expiratory muscle strength training (EMST)
A. Evidence level: low
B. Grade of recommendation: conditional
KQ 7. Compensatory swallowing technique
A.Evidence level: conditional
B.Grade of recommendation: very low
KQ 8. Neuromuscular electrical stimulation (NMES)
KQ 8.1. Swallowing therapy with or without NMES in non-progressive neurological disease
A. Evidence level: moderate
B. Grade of recommendation: strong
KQ 8.2. Swallowing therapy with or without NMES in head and neck cancer
A. Evidence level: low
B. Grade of recommendation: conditional
KQ 8.3. Pharyngeal electrical stimulation (PES) in non-progressive neurological disease
A. Evidence level: low
B. Grade of recommendation: conditional against
KQ 9. Stimulation of the transient receptor potential (TRP) channel with drugs
A.Evidence level: moderate
B.Grade of recommendation: conditional
KQ 10. Biofeedback training
A.Evidence level: low
B.Grade of recommendation: conditional
KQ 11. Specific treatment for cricopharyngeal (CP) dysfunction
KQ 11.1. CP botulinum toxin injection
A. Evidence level: low
B. Grade of recommendation: conditional
KQ 11.2. CP myotomy
A. Evidence level: not applicable
B. Grade of recommendation: expert consensus
KQ 11.3. Balloon dilatation
A. Evidence level: moderate
B. Grade of recommendation: conditional
KQ 12. Swallowing education
A.Evidence level: very low
B.Grade of recommendation: conditional
KQ 13. Noninvasive brain stimulation
KQ 13.1. Transcranial direct current electrical stimulation (tDCS)
A. Evidence level: low
B. Grade of recommendation: conditional
KQ 13.2. Repetitive transcranial magnetic stimulation (rTMS)
A. Evidence level: very low
B. Grade of recommendation: conditional
3. Nutrition for oropharyngeal dysphagia
KQ 14. Tube feeding in patients with suspected long-term dysphagia
A.Evidence level: very low
B.Grade of recommendation: conditional
KQ 15. Modifying food textures
A.Evidence level: very low
B.Grade of recommendation: conditional
KQ 16. Nutritional intervention
A.Evidence level: moderate
B.Grade of recommendation: strong
4. Complications and others
KQ 17. Incidence and mortality rates of aspiration pneumonia
A.Evidence level: high
B.Grade of recommendation: strong
KQ 18. The effect of oral care program
A.Evidence level: moderate
B.Grade of recommendation: strong
KQ 19. The effect of multidisciplinary team approach
A.Evidence level: low
B.Grade of recommendation: conditional
Assessment of oropharyngeal dysphagia
KQ 1. Is early screening effective in improving the prognosis in patients with suspected oropharyngeal dysphagia?
Dysphagia is a medical condition that increases the risk of various complications, such as dehydration, malnutrition, aspiration pneumonia, and airway obstruction, which can lead to serious disability or even death [12-14]. Various methods have been used to screen patients with dysphagia, and it is important to investigate whether early screening tools for dysphagia are effective in improving prognosis and preventing complications that can occur due to dysphagia.
One RCT conducted by Schmidt Leuenberger et al. [12] reported that the incidence of pneumonia decreased in patients who received a clinical assessment of dysphagia (early screening) after pulmonary resection. Ten retrospective studies, including patients with stroke, post extubation dysphagia in an intensive care unit (ICU), and traumatic cervical injuries, showed that respiratory complications were significantly reduced after the early screening of dysphagia [12-21]. Considering that the above studies showed consistent results, early screening is recommended in patients with suspected oropharyngeal dysphagia to reduce the occurrence of pneumonia. If patients with oropharyngeal dysphagia are screened early and are provided with appropriate treatment as early as possible, serious complications, such as pneumonia, can be prevented.
Recommendation
Early screening is strongly recommended in patients with suspected oropharyngeal dysphagia to reduce the occurrence of pneumonia with high levels of evidence.
KQ 2. Is the standardized screening test more effective for the diagnosis of dysphagia than a single screening test?
If screening and appropriate treatments for dysphagia are provided as early as possible, the occurrence of complications related to the disease can be reduced [22]. Various screening tests for dysphagia have been developed and used in clinical practice. Single screening tests, such as the 3-oz water swallow test or the volume-viscosity swallow test, are used, where food is swallowed directly to check the presence of aspiration by coughing, voice change, and change in oxygen saturation [23]. Standardized screening tests, such as the Burke dysphagia screening test (BDST), Gugging Swallowing Screening Test (GUSS), Standardized Swallowing Assessment (SSA), Toronto Bedside Swallowing Screening Test (TOR-BSST), and Clinical Functional Scale for Dysphagia, use a clinical scale by combining various clinical items [24-26].
Shin et al. [23] compared the screening abilities of the single screening test (3-oz water test) and standardized screening tools (GUSS, BDST, and SSA) based on the VFSS findings in patients with stroke. The results showed that there was no significant difference in the screening ability of GUSS compared to other screening tests. Lopes et al. [27] also compared the water test and GUSS and reported that there were no differences in the occurrence of stroke-associated pneumonia, mortality rate, ICU admission rate, and functional status between the two groups. Both studies reported that there was no difference in the accuracy of diagnosis or the occurrence of complications between standardized and single screening tests. However, a standardized screening test tool can evaluate a patient’s swallowing function without directly swallowing food. Therefore, for high-risk patients who cannot swallow their saliva properly, a standardized screening test seems safer than a single screening test that forces them to swallow water.
Recommendation
A standardized screening test may be considered to diagnose dysphagia in patients with suspected oropharyngeal dysphagia (expert consensus).
KQ 3. Is VFSS more effective than clinical evaluation in diagnosing oropharyngeal dysphagia?
Oropharyngeal dysphagia can be evaluated using various clinical assessment tools that can be performed at the bedside, as well as more comprehensive diagnostic tests, such as VFSS, can be applied. VFSS is considered a gold-standard evaluation tool for dysphagia, because it can visualize a series of swallowing processes occurring in the oral, pharyngeal, and esophageal phases [28].
If VFSS is performed in patients with oropharyngeal dysphagia, the presence of dysphagia can be detected more accurately than during a clinical evaluation. Two SRs [29,30] and four studies [31-34] that compared the effectiveness of clinical evaluation and VFSS were identified. Both SRs that included patients with stroke showed that no statistically significant differences were found between clinical evaluation and VFSS in predicting the occurrence of aspiration pneumonia [29,30]. Other studies recommended that VFSS is cost-effective and superior when compared to a clinical bedside swelling evaluation [31-34]. Therefore, clinical evaluation can be useful as an early screening test, and VFSS can be additionally performed to accurately diagnose the presence of dysphagia.
Recommendation
VFSS is strongly recommended for diagnosis of dysphagia with moderate levels of evidence.
KQ 4. Is FEES more effective than VFSS for the diagnosis of dysphagia?
It is necessary to diagnose patients with oropharyngeal dysphagia accurately in order to prevent detrimental complications, such as aspiration pneumonia, and to provide sufficient nutrition as early as possible. In addition, a diagnostic test for dysphagia is necessary to evaluate the recovery of swallowing function before and after treatment.
Diagnostic tests for dysphagia include bedside screening, VFSS, and FESS. VFSS is widely used as a standard diagnostic tool for oropharyngeal dysphagia, and FEES is applied to visualize the swallowing function; it can easily be performed repeatedly, even while lying down. Recently, FEES has been frequently performed to diagnose oropharyngeal dysphagia, and many studies on its usefulness have been reported.
One RCT conducted by Aviv [35] compared the effectiveness of VFSS and FESS in 126 patients with dysphagia. The results showed that there were no statistically significant differences in determining the prevalence of aspiration pneumonia between patients who received FEES and VFSS. A study conducted by Wu et al. [36] reported that FESS was more sensitive in detecting penetration, aspiration, pharyngeal retention, and cough reflex, while Fattori et al. [37] recommended that FESS was useful in visualizing pharyngeal residue. FEES showed superior results in observing airway penetration and pharyngeal residue than VFSS [38,39].
Similar levels of safety and efficacy have been observed between FEES and VFSS in patients with dysphagia. There is no radiation exposure, and it can be easily inspected even in medical institutions that do not have fluoroscopy equipment. The endoscopic swallowing test has a high diagnostic benefit since laryngeal movement can be detected during actual swallowing when dysphagia is suspected. In addition, it has the advantage of being performed repeatedly in various places, and there are no significant complications nor patient discomfort during the procedure. However, it is difficult to observe the whole swallowing process using FEES. The phases of swallowing cannot be assessed, especially the oral phase.
Recommendation
There is insufficient evidence to conclude whether FEES is more effective than VFSS. The two test methods can be performed complementary to each other.
KQ 5. Is oropharyngeal sensory stimulation therapy effective in improving swallowing function and quality of life?
Sensory stimulation therapy is believed to be a potential strategy for treating dysphagia as it activates the peripheral sensory nerves in the larynx and the pharynx to protect the airway from aspiration. It has been reported that the use of NMES can improve swallowing in patients with dysphagia by stimulating the afferent nerves and increasing the sensory input to the central nervous system [40].
A RCT conducted by Maeda et al. [41] showed that 20 patients with oropharyngeal dysphagia who received sensory stimulation showed improvement in oral nutritional intake and functional oral intake scale (FOIS). Zhang et al. [42] also conducted a RCT and compared the effectiveness of the traditional swallowing therapy, sensory approach (NMES on the sensory input) combined with traditional swallowing therapy, and motor approach (NMES on the motor muscle) combined with traditional swallowing therapy. All the groups showed improvement in swallowing function and quality of life after 4 weeks of treatment, but the sensory approach combined with traditional swallowing therapy showed a statistically significant improvement compared to the other groups [42]. Another RCT performed by Rofes et al. [43] showed that after 10 days of treatment with sensory or motor surface electrical stimulation, 20 patients with chronic post stroke dysphagic (10 sensory vs. 10 motor) showed improvement in swallowing function after treatment compared to that before treatment. These studies suggest that oropharyngeal sensory stimulation therapy in patients with oropharyngeal dysphagia may contribute to an improvement in swallowing function and an increase in quality of life.
Recommendation
Oropharyngeal sensory stimulation therapy is recommended in patients with oropharyngeal dysphagia to improve swallowing function and improve quality of life.
KQ 6.1. Are tongue and pharyngeal muscle strengthening exercises effective in improving swallowing function and quality of life, reducing the incidence of pneumonia, and improving quality of life?
Tongue and pharyngeal muscle strengthening exercises are one of the treatment methods for dysphagia. Strengthening exercises are often applied for better lingual and pharyngeal strength and improvement in swallowing ability [44]. These exercises aimed to increase the diameter of the upper esophageal sphincter (UES) opening and decrease post deglutitive aspiration and dysphagic symptoms [45].
Twelve RCTs investigated whether strengthening exercises for the tongue and laryngeal muscles were effective in improving the swallowing function and reducing the incidence of aspiration pneumonia compared to the control group. Three and eight RCTs on patients with brain lesions and head and neck cancer, respectively, were found. These studies applied rehabilitative techniques, such as head lift exercise, Shaker exercise, Mendelsohn maneuver, and muscle strengthening exercises of the tongue and larynx.
Regarding patients with stroke, in a RCT conducted by Kang and Kim [1], patients with dysphagia showed a significant improvement in the neck strength and swallowing function when head lift exercises were performed for 30 minutes, 5 times a week for 6 weeks. RCTs conducted by McCullough et al. [46] and McCullough and Kim [47] also showed that the 2 weeks of the Mendelsohn method training improved hyoid anterior and superior movements and increased UES opening and swallow physiology in 18 patients with stroke and dysphagia. Regarding patients with oropharyngeal cancer, Kotz et al. [48] investigated the effect of prophylactic swallowing exercises in 26 patients with head and neck cancer. This study showed that patients who performed swallowing exercises (five exercises, including effortful swallowing, super-supraglottic swallowing, tongue hold, tongue retraction, and Mendelsohn maneuver, 10 times per day, and three times a day) showed better swallowing outcomes than patients who did not perform the exercises at 3 and 6 months after the treatment [48]. A RCT conducted by Lazarus et al. [44] also showed that tongue-strengthening exercises improved swallowing function in 12 patients with oropharyngeal cancer who underwent radiotherapy compared to 11 patients who were administered only conventional treatment. Notably, other studies also reported similar results.
In summary, tongue and pharyngeal muscle strengthening exercises contribute to improving swallowing function and reducing aspiration pneumonia in patients with brain lesions and head and neck tumors. Since these exercises can be easily performed for inpatients and outpatients in rehabilitation clinics, they are recommended for the treatment of dysphagia.
Recommendation
Tongue and pharyngeal muscle strengthening exercises are recommended to improve swallowing function and reduce the incidence of pneumonia.
KQ 6.2. Is EMST effective in improving swallowing function or quality of life?
The EMST increases subglottic air pressure, while changes in motor unit recruitment and neuromodulation have been proposed as the mechanism of effect.
Four RCTs on EMST showed that it improved swallowing function in patients with dysphagia. Three RCTs on patients with stroke [49-51] and one RCT on patients with multiple sclerosis [52] used commercially available EMST 150 equipment (Aspire Products LLC., Cape Carteret, NC, USA) and compared the effect with the sham treatment. As for EMST, a protocol of five sets per day was applied for 5 days a week. One set included five vigorous exhalations at 70% of the maximum expiratory pressure. All of these studies showed that EMST was effective in improving swallowing function compared to the control group [49-52], and the study conducted by Silverman et al. [52] also reported that it improved swallowing-related quality of life. EMST can improve swallowing function as well as respiratory function in patients with non-progressive neurological disease, thereby contributing to improving swallowing-related quality of life, but it can be only applied to patients who can fully understand the training method. Clinicians should be aware of its side effects, as performing strong expiratory pressure can cause hypotension, hyperventilation, or dizziness.
Recommendation
EMSTs are suggested to improve swallowing function and quality of life.
KQ 7. Are compensatory swallowing maneuvers effective in improving swallowing function, lowering the incidence of pneumonia, and improving quality of life?
Compensatory maneuvers are one of the rehabilitative strategies for dysphagia management. The compensatory swallowing maneuvers aim to keep patients safe when swallowing and promote temporary stability without permanently changing the swallowing mechanism. Compensatory swallowing maneuvers include chin tuck, chin down, head extension, head rotation, effortful swallow, Mendelsohn maneuver, tongue-hold maneuver, or Masako maneuver, supraglottic swallow, and super-supraglottic swallow. Compensatory swallowing maneuvers can induce immediate stability of the swallowing; however, as the same method must be applied every time swallowing occurs, patients may get tired easily due to the repeated application.
According to the observational study conducted by Solazzo et al. [53], compensatory swallowing techniques, such as a chin-down posture, head turned posture, and a hyperextended head posture, promoted safe swallowing in 66 (88.0%) of 75 patients with dysphagia. Furthermore, a study published by Ra et al. [54] also showed the effect of chin tuck, and the study conducted by Miyamoto et al. [55] reported that the chin-down maneuver was beneficial to swallowing function. The evidence for the effect of effortful swallowing seems to be weak at present, and no studies were found regarding the effect of Mendelsohn maneuver and tongue hold maneuver as compensatory swallowing techniques. Regarding supraglottic and super-supraglottic swallowing, a study reported that super-supraglottic swallow changes the airway closure and hyoid-larynx movement [56], while another study reported that supraglottic swallow does not change the propelling pressure of food lumps [57]. Further studies on their direct effect on swallowing function are needed in the future.
Compensatory swallowing maneuvers do not require a large burden of time and cost and can positively affect swallowing function and prevent complications. To date, there has been no RCT studying compensatory swallowing maneuvers; therefore, the level of evidence was considered very low.
Recommendation
The compensatory swallowing technique is suggested to improve the swallowing function.
KQ 8.1. Is surface NMES combined with swallowing therapy better for improving dysphagia in patients with non-progressive neurological disease compared with swallowing therapy alone?
Conventional swallowing therapy includes strengthening exercises for muscles involved in swallowing, compensatory maneuvers, sensory and tactile stimulation, and biofeedback [58]. In 2001, U.S. Food and Drug Administration approved the use of NMES, such as VitalStim® (Chattanooga Group, Hixson, TN, USA), for dysphagia treatment. This treatment method involves attaching electrodes to the skin and transmitting electrical signals to the muscles involved in swallowing to induce contraction.
Various studies evaluated the combined effect of surface NMES, including 10 RCTs [42,59-67] and two non-RCTs [68,69]. In most studies, the combination of NMES and swallowing therapy significantly improved objective and subjective indicators of swallowing function. A RCT conducted by Lee et al. [62] showed that when combined with NMES and conventional swallowing therapy, the FOIS was higher at 3 and 6 weeks after treatment compared to conventional swallowing therapy alone. A RCT conducted by Terré and Mearin [66] reported that the combination of NMES and conventional swallowing therapy improved oral intake function and reduced aspiration in patients with dysphagia. A RCT conducted by Xia et al. [67] also showed that the combination of NMES and conventional swallowing therapy was conducive to recovery from post-stroke dysphagia. Nine out of ten studies showed similar results, reporting that the combination of NMES and conventional swallowing therapy helped improve the swallowing questionnaire scores or swallowing test results more significantly than swallowing therapy alone. This treatment method is considered safe and effective. Therefore, NMES, in conjunction with swallowing therapy, is recommended for the treatment of dysphagia.
Recommendation
The combination of surface NMES and swallowing therapy is recommended for improving the swallowing function in patients with non-progressive neuropathic lesions.
KQ 8.2. Is surface NMES combined with swallowing therapy better for improving dysphagia compared with swallowing therapy alone in patients with head and neck cancer?
Dysphagia after head and neck cancer surgery depends on the type and extent of the damage to the structures removed during surgery. It can also occur after radiation therapy, which induces progressive fibrosis of muscles or soft tissues that leads to progressive dysphagia [70].
For the treatment of dysphagia after head and neck cancer surgery, strengthening exercises of remaining muscles, postural maneuvers, and biofeedback techniques have been used to replace the original functions of the resected structures and minimize the weakening of the muscles [70]. The surface NMES has also been applied as an alternative treatment to strengthen the muscles through direct muscle contractions and prevent the atrophy of denervated muscles.
One RCT and two case-control studies investigated the effectiveness of the combination of NMES and conventional swallowing therapy. A RCT conducted by Ryu et al. [71] showed that NMES combined with traditional swallowing training (14 patients) was superior to traditional swallowing training alone (12 patients) in patients with head and neck cancer. Two case-control studies showed that NMES induced significant scores in the FOIS assessment and the degree of movement in the speed of the hyoid bone [72,73]. The combination of NMES and swallowing therapy is beneficial for improving dysphagia in patients with head and neck cancer.
Recommendation
The combination of surface NMES and swallowing therapy is suggested for improving the swallowing function in patients with head and neck cancer.
KQ 8.3. Does PES improve swallowing function and prevent pneumonia in patients with dysphagia caused by non-progressive neurological disease?
PES, which provides electrical stimulation directly to the pharynx, induces activation of the pharyngeal motor cortex via the corticobulbar pathway [74]. PES aims for cortical plasticity by activating the cerebral motor cortex by transmitting repetitive electrical stimulation into the pharynx.
Five RCTs on the PES compared its effect with sham stimulation [74-78]. Four RCTs reported that PES did not significantly improve the swallowing function or prevent pneumonia [74,75,77,78], while only Jayasekeran et al. [76] reported that PES was safe, reduced aspiration, and improved feeding status. Therefore, evidence of the positive effect of PES on improving swallowing function and preventing pneumonia is lacking.
Recommendation
It is difficult to recommend the application of PES in patients with oropharyngeal dysphagia caused by non-progressive nerve lesions since the effects of improving the swallowing function and preventing pneumonia are not clear.
KQ 9. Is stimulating the TRP channel with drugs effective in improving swallowing function, lowering the incidence of pneumonia, and improving the quality of life in patients with oropharyngeal dysphagia?
Although drug treatment for dysphagia is not currently widely applied in clinical practice, a number of drugs have been studied for their effect of improving swallowing response and preventing airway aspiration. TRP channel is a receptor that converts temperature stimuli into electrical signals and transmits them to the central nervous system. A number of substances, including a TRPV1 agonist (capsaisin) and a TRPM8 agonist (menthol), were used in several studies to induce swallowing responses in patients with dysphagia.
The effect of a capsaicin tablet was compared with a placebo tablet for 4 weeks before meals, and upper respiratory protective reflexes significantly improved in 64 older residents in a nursing home [79]. When TRPV1 agonist (capsaicin 1×10-5 M) was administered for 10 days, the penetration–aspiration scale (PAS) score on the VFSS significantly decreased from 5.23±2.04 to 3±1.47 (p=0.002) [80,81]. The stimulation of TRPV1 improved swallowing safety and shortened the swallow response in older adult patients with oropharyngeal dysphagia. In two RTCs conducted by Cui et al. [82] and Wang et al. [83], capsaicin in conjunction with ice or thermal tactile stimulation was beneficial to the recovery of the swallowing function in patients with stroke and dysphagia. In addition to capsaicin, the effect of menthol (TRPM8 agonist) and piperine (TRPV1/TRPA1 agonist) injection studies on the swallowing function have also been reported [84,85]. Most RCTs (11 out of 12) reported that TRP channel stimulation improved swallowing function in the short term, and four non-RCTs reported that TRP stimulation improved the swallow response and swallowing function.
Currently, little is known about pharmacological approaches for the treatment of oropharyngeal dysphagia. Stimulation of the TRP channel via TRPV agonists (including capsaicin), administered through the oral cavity, oropharynx, or through stimulation of the ear canal, showed improvement in the swallowing function for a short period. However, its long-term use should be further investigated. The administration of a TRPV agonist, such as capsaicin, showed a short-term improvement in the swallowing effect, and it can be easily applied in Korea as capsaicin-rich red pepper is a very common food in Korea. The regular stimulation of the TRP channel seems to promote the recovery of the swallowing function in patients with dysphagia, but a clear standard for the dosage and the long-term use of drugs are needed in the future.
Recommendation
Pharmacological stimulation of the TRP channel is suggested for improving swallowing function.
KQ 10. Is biofeedback training effective for improving swallowing function, lowering the incidence of pneumonia, and improving quality of life?
Biofeedback is a technique that provides biological information to patients in real-time and facilitates normal movement patterns or induces sufficient muscle contractions during muscle-strengthening training [86]. Using biofeedback, the exercise performance is notified to the patients through audio-visual information to empower effective rehabilitation. Neuromuscular biofeedback methods include electromyography (EMG) biofeedback and real-time ultrasound imaging biofeedback. EMG biofeedback measures myoelectric signals through surface electrodes attached to target muscles and converts them into visual and auditory signals to induce sufficient muscle contractions [87].
A RCT conducted by Shin et al. [88] showed that suprahyoid muscle activity improved after 4 weeks of biofeedback training using surface EMG, compared to that before treatment in 45 patients with dysphagia after stroke. The effect of visuoauditory biofeedback is superior to visual biofeedback or self-exercise alone [88]. Another RCT conducted by Moon et al. [89] showed that swallowing training (effortful swallow and Mendelsohn maneuver) with surface EMG biofeedback training was more effective than swallowing training alone. Other case-control studies also showed that surface EMG biofeedback induced improvement in swallowing scores, such as functional dysphagia scale (FDS), PAS, videofluoroscopic dysphagia scale (VDS), or FOIS [90-94].
In summary, swallowing treatment using biofeedback is an effective adjunct to conventional swallowing therapy to improve swallowing function in patients with dysphagia. Although there is not much evidence, the benefit is clear compared to the harm. Since there are many hospitals that do not have biofeedback equipment, if applicable, biofeedback in conjunction with conventional swallowing therapy is recommended.
Recommendation
Biofeedback training is suggested for improving swallowing function.
KQ 11.1. Is CP botulinum toxin injection effective for improving swallowing function, reducing the risk of aspiration pneumonia, and improving diet in patients with CP dysfunction?
The CP muscle, which is located between the throat and esophagus, is the main component of UES. CP dysfunction or impaired relaxation due to various diseases, such as neurological disease, head and neck cancer, and Zenker’s diverticulum, causes symptoms of dysphagia, aspiration, and weight loss [95,96]. In patients with CP dysfunction, the cricopharyngeus fails to open during swallowing. Treatments for CP dysfunction include swallowing therapy and interventional techniques, such as botulinum toxin injection, dilatation, and myotomy. The effectiveness of CP botulinum toxin injection, which was first introduced by Blitzer in 1993, has been reported in previous studies [97].
Several studies reported the effects of CP botulinum injection, including two studies conducted by Alfonsi et al. [98] and Kelly et al. [99], which included 69 and 49 patients with CP dysfunction, respectively. Scores obtained from the eating assessment tool and Dysphagia Outcome and Severity Scale (DOSS) showed improvement after botulinum toxin injection. Botulinum toxin injection was highly effective in the treatment of dysphagia. In the study published by Jeong et al. [100] and Kim et al. [101], the success rate of botulinum toxin injection was 63.9% and 78.6%, respectively. The complication rate was very only, with only one patient showing temporary unilateral vocal fold paralysis [101]. The relative risk of the CP botulinum toxin injection seems to be low, and the benefits seem greater than the harms.
Recommendation
CP botulinum toxin injection is suggested to be performed while carefully considering the characteristics of dysphagia of each patient and the advantages and disadvantages of treatment.
KQ 11.2. Is CP myotomy effective in improving swallowing function, reducing the risk of aspiration pneumonia, and improving diet in patients with CP dysfunction?
CP myotomy is one of the surgical interventions applied for the treatment of CP dysfunction. CP myotomy is a treatment method that induces functional improvement by performing a complete incision of the CP muscle. Two approaches have been developed: the external transcervical approach, which has been performed for a long time, and the endoscopic CP myotomy, which has been performed relatively recently. In patients with defective CP relaxation, adequate oral and pharyngeal propulsion and laryngeal elevation may have a positive effect on improving the swallowing function. However, it has been reported that the effect of CP myotomy is inconclusive for patients who complain of subjective symptoms without clear abnormalities in anatomy and function [102].
McKenna and Dedo [103] conducted a study on the effects of CP myotomy through an external transcervical approach on 47 patients with CP dysfunction in 1992. After surgery, 45% and 30% of patients showed normal and improved swallowing function, respectively, in the clinical symptom evaluation. Brigand et al. [104] showed that among 253 patients with severe dysfunctional pharyngo-esophageal junction who underwent CP myotomy through an external transcervical approach, 75% of patients reported improvement in oropharyngeal. In addition, postoperative complications were observed in 15.8% of the patients, with the most common complications being mucosal break and pulmonary infection. Dauer et al. [105] compared eight patients who underwent CP myotomy through an external transcervical approach and 14 patients who underwent endoscopic CP myotomy. The laser technique was as effective as the transcervical approach, with a low risk of major complications. Takes et al. [106] and Ho et al. [107] showed that most patients reported improvement in dysphagia symptoms after endoscopic CP myotomy at 3 and 6 months, respectively.
Symptomatic improvement after CP myotomy seems to be approximately 60%–70% in patients with CP dysfunction. However, the clinician should consider that CP myotomy is invasive, irreversible, and permanent treatment with a possible risk of complications. Therefore, it seems difficult to judge whether the risks will be significantly higher than the relative risk for benefits, so an individual approach based on the patient’s condition seems necessary.
Recommendation
CP myotomy is suggested to be performed carefully in selective cases who receive refractory to conventional treatment while considering the potential side effects, advantages, and disadvantages of the treatment. An individual approach based on the patient’s condition seems necessary.
KQ 11.3. Is balloon dilatation effective in improving swallowing function, reducing the risk of aspiration pneumonia, and improving diet in patients with CP dysfunction?
Balloon dilatation is a treatment method for CP dysfunction and is known as a relatively safe and efficacious in relieving UES dysfunction [108]. One of the dilatation techniques is the use of bougies, which reduces UES pressure and increases relaxation. Balloon dilatation for CP dysfunction restored UES resting pressure, improved UES relaxation, strengthened pharyngeal propulsion, and improved functional oral intake [108].
A RCT conducted by Wei et al. [109] showed that conventional swallowing therapy with modified balloon dilatation increased the excitability of affected projection and induced better improvement in FOIS compared to conventional swallowing alone at 3 weeks of treatment. When balloon dilatation was compared with laser myotomy, both improved UES opening for at least 6 months after the treatment [110]. Other studies also reported the effectiveness of balloon dilatation for treating CP dysfunction.
Balloon dilatation is a procedure that secures the visual field through an endoscope, and the risk of side effects is not high compared to other interventional procedures. It is considered valuable for treating CP dysfunction, but it is still invasive to a degree and may, therefore, require repeated procedures when CP dysfunction recurs.
Recommendation
Balloon dilatation is suggested to be performed carefully in selective cases that are refractory to conventional treatment, considering the advantages and disadvantages of the treatment. An individual approach based on the patient’s condition seems necessary.
KQ 12. Is the swallowing education program effective for improving swallowing function, reducing the risk of aspiration pneumonia, and improving diet?
For the treatment of dysphagia, various methods, including electrical stimulation therapy and swallowing exercises, are effectively used in clinical practice for the recovery of swallowing function. Recently, the need for a comprehensive swallowing education program that includes an understanding of dysphagia, self-swallowing exercise, and management has been emphasized.
Kang et al. [111] applied a comprehensive bedside swallowing exercise education program for 2 months in addition to the conventional swallowing therapy for patients with stroke and dysphagia. A video recording of the swallowing exercises, including oral, pharyngeal, laryngeal, and respiratory exercises, were played in the ward. These videos led to an improvement in swallowing function, emotional state, and quality of life in the patient group who received swallowing education. Cho et al. [112] also showed that the supervised self-exercise swallowing training program for 4 weeks induced improvement in the VDS in patients with stroke. Mashhour et al. [113] showed that swallowing exercise programs are also effective in patients with dysphagia due to the presence of head and neck tumors during radiation therapy. In addition, Chen et al. [114] confirmed that the swallowing exercise education program was effective in improving emotional dysphagia quality of life 6 months after treatment of oral cavity cancer.
The swallowing education program is effective in improving swallowing function. There is no harm that can be caused by performing the program, and the motivation for participation in the program is necessary to maximize its effect. The swallowing education program can be used as a modality for rehabilitation for patients with dysphagia.
Recommendation
The comprehensive swallowing education program, including self-exercise swallowing training, is suggested for improving swallowing function.
KQ 13.1. Is tDCS effective in improving swallowing function, reducing the risk of aspiration pneumonia, and improving diet?
tDCS, one of the non-invasive brain stimulation treatment methods, aims to induce functional improvement through neuroplasticity by controlling the activity of neural networks in the cortical areas. Positive therapeutic effects of tDCS on the recovery of language, motor, and cognitive function in patients with stroke have been reported in previous studies [115]. Regarding the effect of tDCS on patients with dysphagia, Jefferson et al. [116] first investigated the applicability of anodal tDCS stimulation to the pharyngeal motor cortex, and later, several studies reported the effects of tDCS stimulation on dysphagia after stroke.
In 2011, Kumar et al. [117] conducted a RCT wherein anodal tDCS was applied to the pharyngeal motor cortex area contralateral to the lesion site in patients with dysphagia with subacute stroke. There was a significant difference after anodal tDCS (seven patients) compared with sham tDCS (seven patients) in DOSS scores. Other RCTs also reported that anodal tDCS induced better swallowing function when comparing the effect of anodal tDCS with sham tDCS [118-122]. Most recently, in a RCT conducted by Sawan et al. [123], 20 patients who received anodal tDCS with conventional rehabilitation therapy for 5 days showed significant improvement in the swallowing function (VFSS and DOSS score) compared with 20 patients who received sham tDCS. Another recent RCT conducted by Wang et al. [124] reported a significantly higher improvement in the swallowing function after treating with an anodal tDCS, conventional swallowing rehabilitation therapy and catheter balloon dilatation in patients with CP dysfunction after brainstem stroke.
In tDCS, a weak direct current is used to stimulate the cerebral cortex [125]. tDCS has the advantage that it is easy to apply and safe with relatively few side effects. The side effects of tDCS are mild and include local erythema, tingling, or itching. In conclusion, tDCS applied to the contralateral or bilateral hemispheres is beneficial for the improvement of swallowing function when combined with swallowing therapy in patients with dysphagia.
Recommendation
tDCS is suggested for improving the swallowing function in patients with non-progressive brain lesions.
KQ 13.2. Is rTMS effective for improving the swallowing function and diet, as well as reducing risk of aspiration pneumonia?
rTMS is one of the non-invasive brain stimulation methods that is widely used to induce changes in the activity and neuroplasticity of the brain. In stroke, interhemispheric imbalance is observed with decreased excitability of the ipsilesional hemisphere and increased excitability of the contralesional hemisphere. rTMS directly delivers cortical stimulation. Low-frequency (LF) rTMS decreases cortical excitability, while high-frequency (HF) rMTS increases it. Several studies have investigated the effects of rTMS treatment on dysphagia.
A RCT conducted by Khedr et al. [126] showed that 3 Hz bilateral rTMS (10 minutes for 5 days) led to a significantly greater improvement in the swallowing function compared with sham rTMS in patients with stroke and dysphagia. Kim et al. [127] conducted a RCT to compare HF (5 Hz) ipsilateral rTMS (20 minutes for 10 days), LF (1 Hz) ipsilateral rTMS (20 minutes for 10 days), and sham rTMS in patients with brain injury and dysphagia. The results showed that FDS and PAS scores significantly improved after LF rTMS. Lim et al. [128] reported that both rTMS and NMES were effective for improving dysphagia and no significant differences were found between rTMS and NMES. Both HF and LF rTMS (3 Hz and 1 Hz, respectively) were reported to be effective for dysphagia in a RCT by Du et al. [129]. A study conducted by Park et al. [130] showed that bilateral stimulation was superior to unilateral or sham stimulation in 35 patients with stroke and dysphagia. Similarly, Zhang et al. [131] explained that bilateral rTMS combined with NMES produced higher cortical excitability and better swallowing function recovery compared to unilateral or sham rTMS.
Applying unilateral (LF and HF rTMS over the unaffected and affected hemispheres, respectively) or bilateral rTMS are recommended to improve the swallowing function and induce cortical neuroplasticity in patients with dysphagia. Since rTMS is a relatively new intervention in terms of applicability, additional costs are expected in addition to existing interventions, so cost-resource allocation needs to be considered. In addition, since rTMS treatment is not currently covered by medical insurance benefits, active attention by medical staff and institutional arrangements are needed.
Recommendation
rTMS is suggested for improving swallowing function in patients with non-progressive brain lesions.
KQ 14. Does enteral tube feeding improve the clinical course, survival, or nutritional status of patients who are likely to have oropharyngeal dysphagia for a long period of time?
Under nutrition is common in patients with dysphagia and nutritional status can deteriorate as the disease persists. There are two different methods for enteral tube feeding for patients with severe dysphagia. For nasogastric feeding, a tube is inserted through the nose to supply nutrition to the stomach. During a percutaneous endoscopic gastrostomy (PEG), a tube is inserted through a hole directly into the stomach to supply nutrients. Nutrition supply using a nasogastric tube is the most commonly used non-invasive treatment, but complications such as aspiration pneumonia, reflux esophagitis, and esophageal ulcers caused by mechanical stimulation may occur. Also, a nasogastric tube must be replaced once a month. If nasogastric tube feeding is expected to be required for a long period of time, gastrostomy is recommended. However, gastrostomy is an invasive procedure that can sometimes cause complications, such as inflammation and bleeding in the procedure site. It is still controversial whether feeding through a gastrostomy, rather than maintaining a nasogastric tube, affects the clinical course and mortality of patients.
Six RCTs investigated the effect of early or preventive enteral tube feeding, including one study on patients with stroke and five studies on patients with head and neck cancer. The usefulness of early (within 72 hours after stroke) and prophylactic enteral tube feeding was investigated in patients with oropharyngeal dysphagia due to stroke and head and neck cancer. A RCT conducted by Dennis et al. [132] reported that early enteral tube feeding (early defined as tube feeding within 7 days of admission) was associated with an absolute reduction in risk of death and a reduction in death or poor outcome in 741 patients with stroke. Among the five RCTs conducted on patients with head and neck cancer [133-137], three studies assessing the survival rate did not show an association between the application of early or prophylactic enteral tube feeding and the improvement in survival rate [134,136,137]. However, Silander et al. [134] and Salas et al. [133] reported that prophylactic PEG was associated with significantly fewer malnourished patients over time and improved quality of life at 6 months. These studies showed that early enteral tube feeding showed overall improvement in the clinical course or survival rate in patients with oropharyngeal dysphagia.
Five RCTs studies investigated whether to supply nutrients through nasogastric and gastrostomy tubes when tube feeding is to be maintained for a long period of time [138-142]. In most studies, patients who underwent gastrostomy showed better results in nutritional status, including blood albumin and body weight. A higher frequency of gastrointestinal bleeding, pneumonia, or urinary tract infection was reported in the nasogastric tube group compared to the gastrostomy group [140]. Gastrostomy feeding showed a positive effect on nutritional status and weight gain compared to nasogastric feeding. Gastrostomy tube feeding is likely to bring more benefits than nasogastric tube feeding when enteral tube feeding is required for a long period of time. Therefore, switching to a gastrostomy tube is recommended in patients who need to continue nasogastric tube feeding for a long time.
Since adequate nutrition and prevention of weight loss are very important issues in clinical practice, appropriate enteral tube feeding is recommended for patients who need sufficient nutrition. If it is likely that nasogastric tube feeding will continue for a long time, selecting an appropriate candidate who would benefit from gastrostomy tube feeding is recommended.
Recommendation 14-1
In patients who are likely to have oropharyngeal dysphagia for a long period of time, early enteral tube feeding is suggested for improving the clinical course, survival rate, and neurological prognosis.
Recommendation 14-2
In patients who are likely to have oropharyngeal dysphagia for a long period of time, a gastrostomy tube feeding is suggested for improving the clinical course, survival rate, neurological prognosis, and nutritional status.
KQ 15. Does texture modification of food or liquid affect the clinical course (nutrition status or dehydration) of dysphagia?
In patients with oropharyngeal dysphagia, aspiration may occur when food is not controlled in the oral cavity during the oral phase or when an appropriate pharyngeal swallowing response is not initiated during the pharyngeal phase. If the muscle strength of the oral muscles is reduced or coordinated movements for swallowing are not appropriately performed, bolus formation or oral transit of food becomes difficult. In particular, in the case of oropharyngeal dysphagia caused by neurogenic problems, the risk of aspiration of low-viscosity food, such as water, is high due to lack of bolus control, reduced lingual propulsion, or delayed swallowing response in the pharyngeal phase [143]. Aspiration occurring during swallowing can cause poor nutritional status and impede sufficient fluid intake, increasing the risk of aspiration pneumonia [144]. Therefore, texture modification is one of the compensatory strategies for the treatment of dysphagia.
Five RCTs reported the beneficial effect of texture modification for preventing aspiration or aspiration pneumonia. A RCT conducted by Diniz et al. [145] reported that the use of a spoon-thick consistency reduced the risk of aspiration compared with the liquid consistency in 61 patients with stroke and dysphagia. Kyodo et al. [146] suggested that pureed diets containing a gelling agent might reduce the risk of aspiration pneumonia possibly by decreasing pharyngeal residues in patients with moderate to severe dysphagia.
In contrast, Robbins et al. [147] reported that texture modification did not affect the incidence of aspiration pneumonia. In 515 patients with dementia and Parkinson’s disease who presented aspiration on a liquid diet, the 3-month cumulative incidence of pneumonia did not show any difference when texture modification (nectar or honey) was applied compared to chin-down posture. More patients who had thickened liquids showed dehydration, urinary tract infection, and fever compared to those who ingested liquid with the chin-down posture.
There were differences in disease conditions, texture modification settings, and outcome scales among the studies; however, the positive effects of texture modification on the clinical course for patients with dysphagia seem to be significant, especially for the reduction of the risk of aspiration. Texture modification is relatively easy to apply and does not require large costs; therefore, applying texture modification is recommended based on the severity of dysphagia.
Recommendation
Texture modification of food and fluids is suggested based on the severity of dysphagia to improve the clinical course (nutrition status or dehydration) of patients with oropharyngeal dysphagia.
KQ 16. Does nutrition intervention improve intake or nutritional status in patients with oropharyngeal dysphagia?
Nutrition intervention is a process related to setting specific goals to solve the patient’s nutritional problems and establishing and executing plans for nutrition management. It aims to improve the quality of life by inducing changes in eating behavior and improving the patient’s nutritional status [148]. Patients with stroke often show malnutrition after hospitalization, which is presented by a reduction in muscle mass, low body mass, and low serum protein levels. Impaired oral function and dysphagia are associated with decreased oral intake, which increases the risk of malnutrition [149]. Nutrition intervention can reduce complication rates, admission rates, length of hospital stay, cost of care, and mortality [150]. Thus, a multidisciplinary team approach addressing nutritional problems can help patients with oropharyngeal dysphagia.
Eight studies [149,151-157] assessing the effectiveness of nutrition intervention in patients with dysphagia, including three RCTs and five non-randomized intervention studies, were found. A RCT conducted by Germain et al. [151] showed that older patients who received a dysphagia-specific nutrition care program showed significant differences in weight and calorie and protein intake compared to the control group. Reyes-Torres et al. [152] also reported that patients with dysphagia showed increased body weight, consumption of energy and protein, and handgrip strength after a 12-week nutrition intervention (modified consistency diet with a nectar or pudding viscosity) compared to the control group. Another RCT conducted by Taylor and Barr [153] showed that nutrition intervention (small and frequent meals) was associated with increased fluid intake. Five more observational studies showed some or no statistically significant differences in intake and nutritional status after a nutrition intervention; however, overall, nutrition intervention seems positively affect patients with dysphagia.
Recommendation
Nutrition intervention is suggested for improving intake or nutritional status in patients with oropharyngeal dysphagia.
KQ 17. Are the incidence and mortality rates of aspiration pneumonia higher in patients with oropharyngeal dysphagia compared with those without oropharyngeal dysphagia?
Pneumonia is the third leading cause of death in all age groups in Korea, and it is continuously increasing with aging [158]. Aspiration pneumonia is a bacterial pneumonia caused by aspiration of the contents of the oropharynx or upper gastrointestinal tract colonized by pathogenic bacteria and is more severe than non-aspiration pneumonia. It has been reported that aspiration pneumonia accounts for approximately 14.2% of community-acquired pneumonia; it is more common in older adults, requires more frequent ICU treatment, and has a longer hospital stay compared to non-aspiration pneumonia [159]. A major risk factor for aspiration pneumonia is known as dysphagia. Dysphagia is frequently observed in vulnerable patient groups, such as older adults and patients with neurological diseases, and is associated with an increase in mortality rate, hospitalization period, and medical costs [159-163]. Therefore, it is necessary to identify the relationship between dysphagia and aspiration pneumonia and diagnose and monitor high-risk groups to provide appropriate treatment quickly and accurately.
According to the study by Lo et al. [164], which compared 6,979 newly diagnosed patients with dysphagia and 20,937 undiagnosed patients, the incidence of aspiration pneumonia (1.75% vs. 0.92%, p<0.0001) and mortality (23.83% vs. 13.39%, p<0.001) was higher in the dysphagia group than in the control group. The incidence of 1-, 3-, and 5-year aspiration pneumonia and 1-, 3-, and 5-year mortality rates after stroke diagnosis was also higher in patients with dysphagia compared to the control group [160]. Another study also reported that among 9,930 adults aged 65 years or older who were admitted to 1,121 facilities, the presence and severity of dysphagia were related to the occurrence of aspiration pneumonia. Patients diagnosed with aspiration pneumonia had a statistically significant decline in swallowing function within 3 months compared to patients without a diagnosis (32.8% vs. 5.7%, p<0.001) [165]. In addition, other studies reported that the presence and severity of dysphagia were reported to be related to the occurrence of aspiration pneumonia [166-168].
In summary, oropharyngeal dysphagia increases the risk of aspiration, and patients with oropharyngeal dysphagia have a higher incidence and mortality of aspiration pneumonia than those without dysphagia.
Recommendation
The incidence and mortality of aspiration pneumonia are higher in patients with oropharyngeal dysphagia than in those without dysphagia. Therefore, patients with dysphagia should watch out for the occurrence of pneumonia.
KQ 18. Is the oral care program effective for improving oral health and food intake?
Clean hygienic conditions in the oral cavity prevent dental caries and dryness and improve oral health and swallowing by improving oral sensation and salivation. Normal oral swallowing function can prevent swallowing problems at the pharynx stage by properly pulverizing and mixing food and saliva to form an appropriate mass that passes into the pharynx [169,170].
A RCT conducted by Chen et al. [171] showed that patients who received the oral care program showed significant improvement in the oral health assessment tool but not in FOIS compared with patients who had usual oral care. Chipps et al. [172] also conducted a RCT and showed that bacteria colonization decreased after the oral care program. Only two studies were found on the effectiveness of the oral care program; however, overall, it seems that there are no potential risks or side effects in the process of the oral care program, and it is easy to perform. Applying the oral care program can reduce bacterial colonization in the oral cavity and improve oral health and swallowing function.
Recommendation
The oral health care program is recommended for improving oral health and food intake in patients with oropharyngeal dysphagia.
KQ 19. Is the multidisciplinary team approach (doctor, nurse, therapist, nurse, etc.) effective for reducing complications (such as mortality, pneumonia, and other respiratory infections) in patients with oropharyngeal dysphagia?
The multidisciplinary rehabilitation team is made up of health care professionals who work collaboratively with patients and caregivers to evaluate and manage dysphagia. In the multidisciplinary team, doctors, speech-language pathologists, nutritionists, and nurses are usually involved. Prosthodontists and dentists can sometimes also be involved in identifying structural problems related to swallowing, and social workers can be involved in discharge plans. The goal of the multidisciplinary team approach is to identify patients at risk for dysphagia, evaluate the severity of dysphagia, and provide appropriate treatment [173-175].
A RCT conducted by Zheng et al. [176] showed that swallowing function significantly improved in patients with acute stroke who received a multidisciplinary team approach compared to the controls who received the conventional treatment. In four observational studies, patients who received care via the multidisciplinary team approach showed a significantly lower risk of dysphagia, pneumonia, and requirement for respiratory support, as well as greater patient satisfaction regarding swallowing function than patients who received conventional treatment [149,177-179].
Although the level of evidence is low, the multidisciplinary team approach should be performed because it can contribute to the improvement of swallowing function and reduce the occurrence of pneumonia. Overall, the multidisciplinary team approach seems to be effective in reducing the incidence of pneumonia during rehabilitation treatment of dysphagia.
Recommendation
A multidisciplinary team approach (doctors, nurses, therapists, etc.) is suggested for preventing complications (such as mortality, pneumonia, and other respiratory infections) in patients with oropharyngeal dysphagia.
DISCUSSION
This CPG aimed to review the literature and provide evidence-based guidelines for the assessment and management of dysphagia. This guideline is intended to help medical staff and related subjects in charge of patients with oropharyngeal dysphagia to make safer and more effective decisions by presenting assessment and treatment guidelines based on scientific and objective evidence. Therefore, this guideline aims to effectively deliver the information necessary for decision-making and provide patients with dysphagia with appropriate education, evaluation, and treatment. This will enable patients to improve their symptoms of dysphagia and improve their quality of life. The ultimate goal is to reduce complications and mortality due to the presence of dysphagia.
First, the effectiveness of diagnostic testing for oropharyngeal dysphagia was assessed. Early screening was effective in patients with suspected oropharyngeal dysphagia to reduce the occurrence of pneumonia with a high level of evidence. The recommendation levels were strong, and we concluded that if patients with oropharyngeal dysphagia are screened early and are provided with appropriate treatment as early as possible, serious complications, such as pneumonia, can be prevented. Standardized screening tests, such as BDST, GUSS, SSA, TOR-BSST, or Clinical Functional Scale for Dysphagia, were effective in diagnosing dysphagia, as well as single screening tests, such as the 3-oz water swallow test or the volume-viscosity swallow test. For high-risk patients who are unable to swallow their saliva properly, a standardized screening test was safer than a single screening test, which requires swallowing water. A standardized screening test tool can evaluate a patient’s swallowing function without directly swallowing food, and it was recommended to diagnose dysphagia in patients with suspected oropharyngeal dysphagia. To visualize a series of swallowing processes occurring in the oral, pharyngeal, and esophageal phases, and detect dysphagia, VFSS was strongly recommended for diagnosis of dysphagia with moderate levels of evidence. FEES can also be used to visualize the swallowing function, but FEES does not seem to be more effective than VFSS. Considering the benefits of the two diagnostic methods, we concluded that the two test methods complement each other and can be performed together.
There are various treatment methods for managing dysphagia. We investigated the efficacy of various rehabilitative strategies that are commonly used for the treatment of dysphagia. Oropharyngeal sensory stimulation therapy was effective in improving swallowing function and quality of life, as well as tongue and pharyngeal muscle strengthening exercises, which improved the swallowing function and reduced aspiration pneumonia in patients with brain lesions and head and neck tumors. EMSTs were also effective in improving the swallowing function and quality of life. Compensatory maneuvers, including chin tuck, chin down, and effortful swallow, were useful for improving the swallowing function and were recommended as effective rehabilitative techniques for dysphagia management. The combination of NMES and swallowing therapy was also recommended for improving the swallowing function in patients with non-progressive neuropathic lesions and head and neck cancer. The efficacy of PES for improving swallowing function and preventing pneumonia was unclear.
Treating dysphagia with drugs by stimulating the TRP channel, such as capsaicin, menthol, or piperine, was effective for improving the swallowing function, although it is well applied in clinical practice. Thus, future studies should investigate the effect of drug treatment. In addition, swallowing treatment using biofeedback as an adjunct to conventional swallowing therapy was effective in improving swallowing function. CP botulinum toxin injection, CP myotomy, and balloon dilatation seem to be effective treatment options for patients with CP dysfunction but should be performed after considering the advantages and disadvantages of the treatments. The effect of non-invasive brain stimulation treatment methods, such as tDCS and rTMS, were also investigated, and both of them were effective in improving the swallowing function in patients with non-progressive brain lesions.
As for the nutrition issues, we concluded that early enteral tube feeding improved the clinical course, survival rate, and neurological prognosis for patients who are likely to have oropharyngeal dysphagia for a prolonged period. In addition, gastrostomy tube feeding should also be considered to improve the clinical course, survival rate, neurological prognosis, and nutritional status in patients who are likely to have oropharyngeal dysphagia for an extended period. In addition, texture modification of food and fluids based on the severity of dysphagia improved the clinical course of patients with oropharyngeal dysphagia, especially in reducing the risk of aspiration. Nutrition intervention, including addressing nutritional problems and establishing plans for nutrition management, was recommended because a literature search showed that ithelps improve intake or nutritional status in patients with oropharyngeal dysphagia.
Other issues associated with dysphagia have also been addressed in this CPG. The current evidence showed that the incidence and mortality of aspiration pneumonia were, in fact, higher in patients with oropharyngeal dysphagia than those without dysphagia. Providing the oral health care program improved oral health and food intake in patients with oropharyngeal dysphagia. Additionally, a multidisciplinary team approach, including doctors in various fields, nurses, and therapists, was effective in preventing complications (such as mortality, pneumonia, and other respiratory infections). Various methods for the treatment of dysphagia should be performed, considering various aspects in patients with oropharyngeal dysphagia.
This CPG has several limitations. First, the statistical significance was not evaluated, and meta-analysis was not performed. Second, although the level of evidence for each clinical question was established based on the results of studies abroad, the recommendations of this CPG were primarily based on the applicability of the resources and healthcare system in Korea.
In conclusion, this CPG is the first guideline that provides the levels of evidence of relevant literature and the consensus of multidisciplinary experts regarding issues related to oropharyngeal dysphagia. Physicians, patients, caregivers, and other healthcare professionals are expected to widely read this CPG to improve their understanding and treatment of dysphagia.
Notes
The members who were involved in this guideline had no other conflicts of interest (COI). The COI was required to determine whether or not these persons should be involved in the development of similar guidelines, employment, financial interests, and other potential interests. No potential conflicts of interest relevant to this article were reported.
Acknowledgements
This guideline was developed with financial support from the Korean Academy of Rehabilitation Medicine and the Korean Dysphagia Society. The development of this CPG was not influenced by the supporting academies and was not supported by other groups.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.5535/arm.23069.
Summary of current evidence of neurodevelopmental assessment tool
Supplementary Data 1.
Search strategy
Supplementary Data 2.
Evidence table and risk of bias

